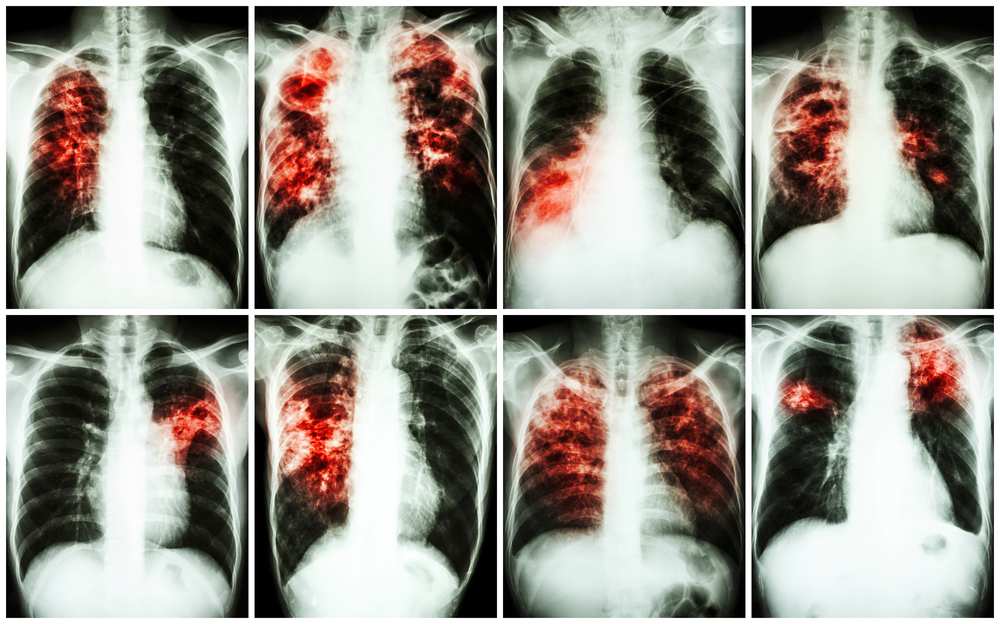
Respiratory diseases are a major cause of morbidity and mortality.
The magnitude of the problem is staggering. Hundreds of millions of people are burdened with chronic respiratory conditions. Four million people die prematurely from chronic respiratory diseases each year1 2, and 90% of these deaths occur in low- and middle-income countries.
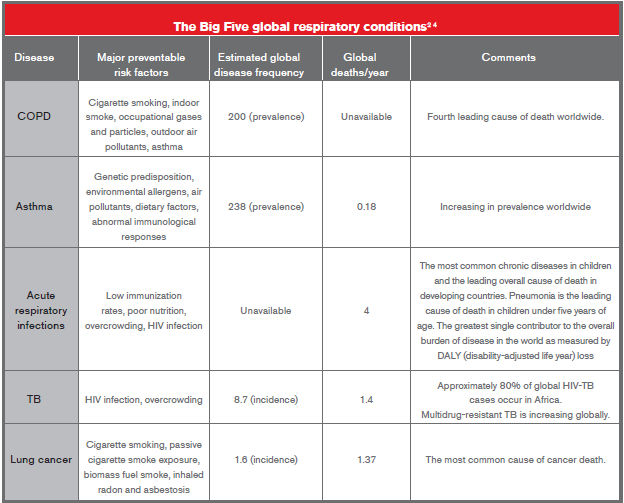
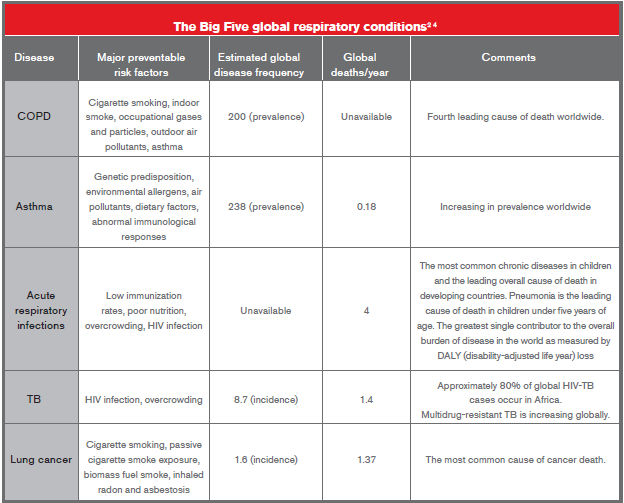
Developed countries experience high levels of asthma, chronic obstructive pulmonary disease (COPD) and lung cancer3. In developing countries, major problems include tuberculosis (TB) and other respiratory system infections. Four external, modifiable drivers are responsible for a substantial percentage of the disease burden represented by the major lung diseases: tobacco, outdoor air pollution, household air pollution, and occupational exposures to lung toxins. The Forum of International Respiratory Societies, in its recent report entitled “Respiratory Disease in the World: Realities of Today – Opportunities for Tomorrow,” identified five conditions that are primary contributors to the global burden of respiratory disease: asthma, chronic obstructive pulmonary disease, acute respiratory infections, tuberculosis, and lung cancer4.
Acute Respiratory Infections
Respiratory infections account for more than four million deaths annually and are the leading cause of death in developing countries5. Respiratory tract infections are caused by many viral and bacterial pathogens6 and are the second most common cause of morbidity and mortality worldwide7 8 9. Lower respiratory tract infections come second in the Global Burden of Disease (GBD) rankings, after ischemic heart disease6 9.
The emergence of difficult-to-treat known and novel bacterial, viral, and fungal respiratory tract pathogens with epidemic potential is of major global concern. The past century has seen several epidemics of new viral respiratory tract infections, most of which emerged from interactions between people and animals10. Some of these include severe acute respiratory syndrome coronavirus (SARS-CoV), avian influenza viruses H5N1, H7N9, and H10N8, variant influenza virus A H3N2, swine-origin influenza virus A H1N1, human adenovirus type 14, and the Middle East respiratory syndrome coronavirus (MERSCoV). Unfortunately these microorganisms do not respect international boundaries, and ease of global travel and airborne spread make them a persistent threat to global health security11.
Pneumonia is the most common acute respiratory infection. In children under five years of age, pneumonia accounts for 18% of all deaths, or more than 1.3 million annually12, and kills far more than HIV or malaria5. Pneumonia occurs several-fold higher in the elderly and HIV-infected individuals. Streptococcus pneumonia remains the most frequent bacterial cause of pneumonia. Pneumonia can also lead to chronic respiratory diseases such as bronchiectasis.
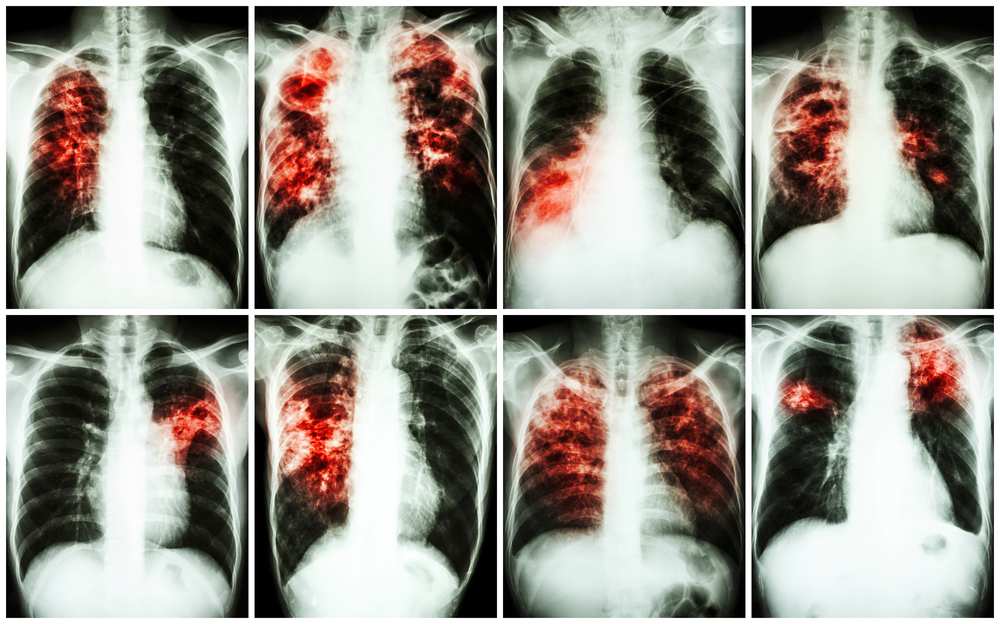
Tuberculosis
Tuberculosis causes about 1.3 million deaths every year13. Globally, about three million cases of tuberculosis every year remain undiagnosed and these infected individuals continue to spread the disease, especially in high-burden TB countries such as Cambodia13, China13, India40, the Philippines13 and Vietnam13. Though the global incidence of drug-susceptible tuberculosis is declining, the emergence of multidrug-resistant (MDR) and extensively drug-resistant (XDR) tuberculosis during the past decade is threatening to reverse this trend. This is further complicated by co-morbid infections, especially HIV, mainly in Africa. Nearly half a million cases of multidrugresistant tuberculosis are diagnosed worldwide every year and a third of patients with this disease will die because of failure of diagnosis or unavailability of appropriate treatment13.
The World Health Organization has set the goal of eliminating TB by the year 2050. Efforts in its global Stop TB strategy has led to advances in TB diagnostics and drugs and, to a lesser extent, TB vaccines. Two diagnostics which have made significant advancement are the Xpert MTB/RIF assay nucleic acid simplification test, for simultaneous detection of mycobacterium tuberculosis DNA and rifampicin resistance in sputum14 and the detection of mycobacterial cell wall lipoarabinomannan (LAM) in urine to diagnose tuberculosis in patients with advanced HIV disease15. Several new effective antimicrobials, including delamanid, bedaquiline, and linezolid, have recently become available for clinical use, but a combination regimen for drug-resistant tuberculosis needs urgent validation in a prospective clinical study in intermediate-burden and high-burden settings16.
Asthma
Asthma is a common chronic non-communicable disease that affects as many as 334 million people of all ages in all parts of the world17. It is concerning that the global burden of asthma, which is already substantial in terms of both morbidity and economic costs, seems to be increasing rapidly as the world becomes more westernized. The recent Global Burden of Disease study estimated that asthma was the 14th most important disorder in terms of global years lived with disability. Currently, 14% of the world’s children and 8.6% of young adults (ages 18-45) experience asthma symptoms, and 4.5% of young adults have been diagnosed with asthma and/or are being treated for asthma. The burden of asthma is greatest for children of ages 10-14 and the elderly of ages 75-7918.
Though the prevalence of asthma is increasing, evidence suggests that asthma mortality and health care utilization rates continue to plateau and/or decrease. The number of deaths due to asthma in 2009 was approximately 27% lower than
the number of deaths in 199919. The number and rate of hospital discharges also both decreased by 24% between 2003 and 201020.
Asthma has global distribution, with a relatively higher burden of disease in Australia and New Zealand, some countries in Africa, the Middle East and South America, and northwestern Europe. Environmental factors are much more likely than genetic factors to have caused the large increase in the numbers of people in the world with asthma.
Chronic Obstructive Pulmonary Disease (COPD)
It is estimated that there are at least 210 million persons in the world with COPD, and that this group of conditions causes three million deaths annually4. The disease burden from COPD appears to be growing despite the development of new therapeutics such as long-acting anti-muscarinic agents, long-acting betaagonists, inhaled corticosteroids, and phosphodiesterase inhibitors.
COPD is now the third leading cause of death in the world21 23. This is much earlier than the predicted ranking by 2030 as per the World Health Organization. The burden of COPD is projected to increase substantially in Asia and Africa in the coming decades, mostly as a result of increased tobacco use in those regions21.
More than 1.1 billion people worldwide smoke, with 82% of smokers residing in low- and middle-income countries22. Although many high-income countries have witnessed decreases in smoking rates, overall smoking prevalence has continued to increase in many low- and middle-income countries24. Tobacco smoking is a well-established major risk factor, but emerging evidence suggests that other risk factors are important, especially in developing countries. As an estimated 25% of patients with COPD have never smoked, the burden of non-smoking COPD is much higher than previously believed. About three billion people, half the worldwide population, are exposed to smoke from biomass fuels compared with 1.01 billion people who smoke tobacco, which suggests exposure to smoke from the burning of biomass fuels might be the biggest risk factor for COPD globally25.
Lung Cancer
Lung cancer has been the most common cancer in the world for several decades. There are estimated to be 1.8 million new cases in 2012 (12.9% of the total), 58% of which occurred in the less developed regions. The disease remains as the most common cancer in men worldwide (1.2 million, 16.7% of the total) with the highest estimated age-standardized incidence rates in Central and Eastern Europe (53.5 per 100,000) and Eastern Asia (50.4 per 100,000). Notably low incidence rates are observed in Middle and Western Africa (2.0 and 1.7 per 100,000 respectively). In women, the incidence rates are generally lower and the geographical pattern is a little different, mainly reflecting different historical exposure to tobacco smoking. Thus the highest estimated rates are in North America (33.8) and Northern Europe (23.7) with a relatively high rate in Eastern Asia (19.2) and the lowest rates again in Western and Middle Africa (1.1 and 0.8 respectively)26.
Lung cancer is the most common cause of death from cancer worldwide. It is estimated to be responsible for nearly one in five deaths (1.59 million, 19.4% of the total). Additionally, lung cancer survival rates continue to be poor27 28. Age-adjusted
lung cancer death rates in the U.S. over a period of six decades shows a declining trend in males whereas females show a rising trend, mainly because of the decline in smoking among males and a concurrent increase in smoking among females27. Because of its high fatality (the overall ratio of mortality to incidence is 0.87) and the relative lack of variability in survival in different world regions, the geographical patterns of mortality closely follow those of incidence26.
Due to lung cancer's high mortality, various controlled trials of screening for lung cancer using sputum examinations, chest radiography or chest CT (computed tomography) scans have been carried out. The current evidence does not support screening for lung cancer with chest radiography or sputum cytology. Annual low-dose CT screening is associated with a reduction in lung cancer mortality in high-risk smokers, but further data are required on the cost effectiveness of screening and the relative harms and benefits of screening across a range of different risk groups and settings29.
Though not one of the Big Five, respiratory diseases remain incomplete without the mention of interstitial lung disease (ILD). More than 300 different conditions are included among the total number of ILDs.The most important ILDs are sarcoidosis, idiopathic pulmonary fibrosis (IPF) (previously called cryptogenic fibrosing alveolitis, mainly in the U.K.), extrinsic allergic alveolitis, ILD as a feature of connective tissue disorder, drug-induced ILD and pneumoconiosis. Data from ILD registries show that the most frequent ILDs are IPF and sarcoidosis, which together comprise about 50%30. IPF is the most common and severe form of idiopathic interstitial pneumonia (IIP). It is irreversible, has an unpredictable and variable clinical course and is associated with extremely poor prognosis, with a death rate worse than that of many cancers (three-year survival, 50%)31 32 33.
There are no large-scale studies of the incidence or prevalence of IPF on which to base formal estimates. A study from the U.K. reported an overall incidence rate of only 4.6 per 100,000 person-years, but estimated that the incidence of IPF increased by 11% annually between 1991 and 200334. This increase was not felt to be attributable to the aging of the population or increased ascertainment of milder cases. Another study from the U.S. estimated the incidence of IPF to be between 6.8 and 16.3 per 100,000 persons, using a large database of healthcare claims in a health plan35.
Prevalence estimates for IPF have varied from 2 to 29 cases per 100,000 in the general population. The wide range in these numbers is likely explained by the previous lack of a uniform definition used in identifying cases of IPF, as well as by differences in study designs and populations. It is unknown if the incidence and prevalence of IPF are influenced by geographic, ethnic, cultural, or racial factors.
Mortality rates for pulmonary fibrosis (PF) increased steadily in the U.S., England and Wales, Scotland, Australia, and Canada from the late 1970s to the early 1990s. A U.S. study showed that mortality rates from pulmonary fibrosis further increased from 1992 to 2003. With the advent of better diagnostic facilities and improved overall life expectancy, incidence of ILD will most likely continue to further increase36.
A study published in October 2014 revealed that mortality from IPF is also increasing steadily worldwide. It is estimated that in 2014, there will have been between 28,000 and 65,000 deaths in Europe and between 13,000 and 17,000 deaths in the U.S. Increasing mortality rates may be due to true increases in incidence, but some of the trends may relate to changes in diagnostic or coding practices37.
After years of ineffective treatment, two new drugs – pirfenidone and nintedanib – have shown promise for patients with IPF38 39.
Conclusion
Insurers are seeing increasing numbers of applicants and claimants with respiratory diseases. Scientific advances over the past several years have been reducing mortality from asthma, acute respiratory infections and other conditions. Interacting environmental factors, however, are generating substantial increases in global incidence trends for the more severe chronic respiratory diseases: asthma, COPD, interstitial lung disease and drug-resistant tuberculosis. These are substantially increasing morbidity trends as well as health care costs. Knowing these global trends will be useful in life underwriting and for underwriting living benefits such as CI, TPD, IP and Hospitalization.
Summary
- The Big Five contributors to the global burden of respiratory disease are: asthma, chronic obstructive pulmonary disease, acute respiratory infections, tuberculosis and lung cancer.
- Respiratory tract infections are the second most common cause of morbidity and mortality worldwide. Pneumonia is the most common serious respiratory infection in children under five years of age, accounting for 18% of all deaths.
- Although the global incidence of drug-susceptible tuberculosis is declining, the emergence of multi-drugresistant (MDR) and extensively drug-resistant (XDR) tuberculosis strains during the past decade are threatening to reverse this trend.
- Mortality from asthma as well as hospitalization due to asthma is decreasing, but the prevalence of asthma is increasing. Asthma is the 14th most important disorder in terms of global YLDs (years lived with disability).
- COPD is now the third leading cause of death in the world. Interestingly, 25% of COPD patients have never smoked.
- Lung cancer is the most common cause of death from cancer worldwide. Annual low-dose CT screening is associated with a reduction in lung cancer mortality in high-risk smokers.
- Mortality from idiopathic pulmonary fibrosis, one of the most frequently found interstitial lung diseases, has been increasing steadily worldwide. This might be due to true increases in incidence, but could also be due to changes in diagnostic and/or coding practices.