In the world of mental health disorders, depression is a commonly encountered condition that in its chronic form may present significant mortality, morbidity and socioeconomic challenges.
Mental health disorders involve disturbance in thinking, emotion and/or behavior. Although considerable advancements have taken place over the years in terms of diagnosis and treatment of mental health disorders, social stigma still persists around them and depression is no exception. Individuals diagnosed with depression may believe that other individuals consider depression as a sign of weakness. Therefore, besides personal struggle, individuals with depression also have to battle societal perceptions of depression – many of which are incorrect or unfounded.
The aim of this article is to update readers on the understanding of the disease process and advances in the treatment and prognosis of depression (unipolar/major), as well as to address the underwriting implications for life and health insurers.
Epidemiology and types of depression
Depression, also known as major depressive disorder or clinical depression, is a common mental health disorder with worldwide incidence. Characterized by low mood, loss of interest and reduced energy, it causes varying levels of social and occupational dysfunction.1
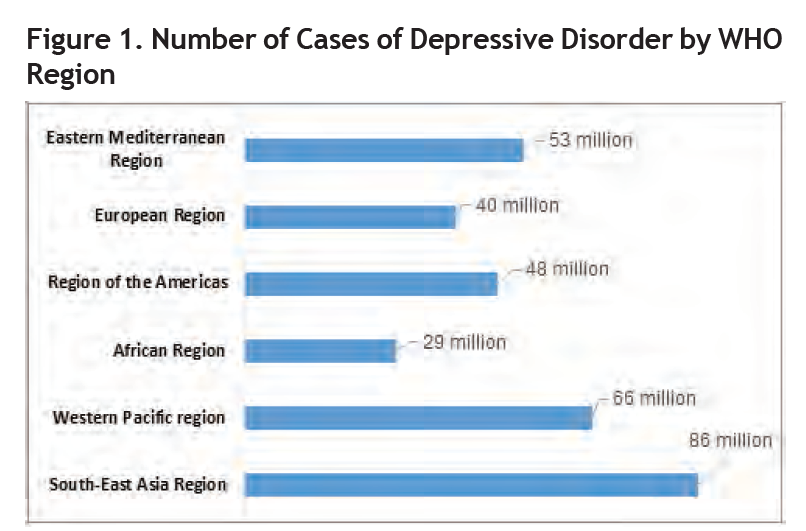
The World Health Organization (WHO) estimates that more than 300 million people suffer from depression worldwide.2 Furthermore, from 2005 to 2015 there was a significant increase, around 18%, in the number of people living with depression. (Figure 1).
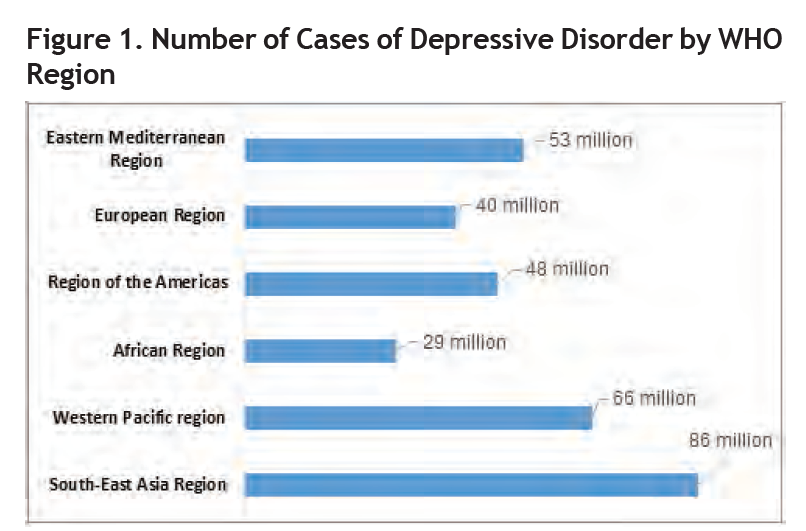
Source: Adapted from www.who.int/news-room/fact-sheets/detail/depression.
Depression can occur at any age. However, the majority of affected individuals are women, the young and elderly populations.4,5
Two of the most common forms of depression are as follows:6,7
Some other forms of depression develop under unique circumstances and include:
- Seasonal affective disorder – depression that may come and go with the seasons.
Perinatal (postpartum) depression – depression that may develop during pregnancy or after delivery.
Psychotic depression – depression with some form of associated psychosis.
Premenstrual dysphoric disorder (PMDD) – depressive symptoms or tension before menstruation.
Substance/medication-induced depressive disorder.
Etiology and manifestations
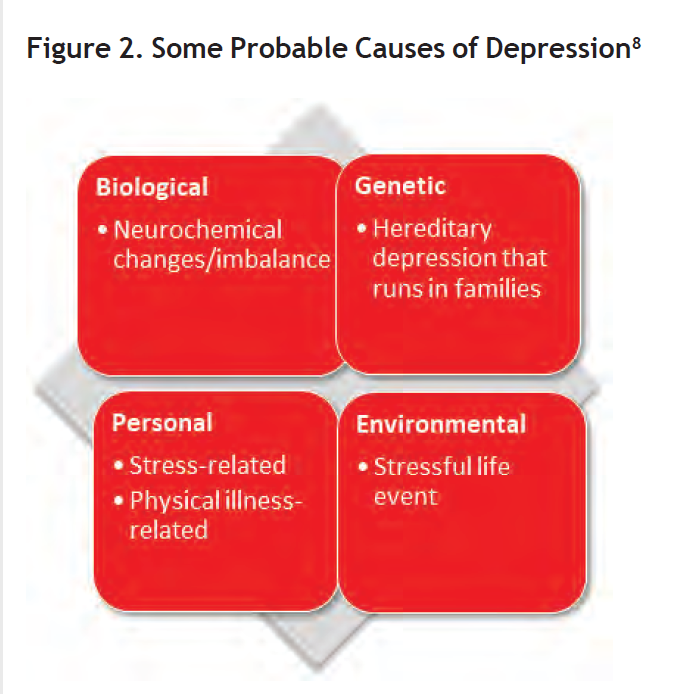
Depression is a complex mental disease without any specific cause. However, there are multiple factors that overlap with one another and can result in the occurrence of depression. (Figure 2)
Source: Adapted from www.nhs.uk/conditions/clinical-depression/causes/.
In addition to these etiological factors, certain other triggers such as low self-esteem, previous episode(s) of depression, and drug or alcohol abuse may play an augmenting role in the incidence of depression.
Recurrent or chronic depression can be more than a constant state of sadness, which subsequently has a profound impact on an individual’s physical and mental health. Although depression can manifest differently in men, women and children, the relevant symptoms can be summarized below in accordance with the Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5):
- Depressed mood, headaches.
- Loss of pleasure.
- Irritability.
- Inability to concentrate.
- Insomnia, restless sleep or excessive sleepiness at times.
- Fatigue, decreased energy.
- Change in appetite, weight changes.
- Withdrawal from social engagements.
- Thoughts of suicide, self-harm.
Given the nature of the disorder, the symptoms may vary based on the underlying etiology, and the greater the number of symptoms present, the greater the likelihood of severe disease. In addition, individuals with chronic or severe physical disorders such as cancer and heart attack, or with physiological processes like pregnancy or menopause, may mimic symptoms similar to depression. Symptoms of depression may also overlap with other existing or underlying mental health conditions. Hence, an accurate evaluation of symptoms is important in differentiating and classifying depression from other mental and physical health disorders.
Investigation and diagnosis
The correct identification of depression is critical to minimizing patient distress, as well as ensuring that the proper treatment is delivered in an expedient manner.
Currently, no laboratory tests exist to assess depression, and the administration of clinical evaluation and standardized interviews to assess depression can be compromised by poor patient reporting and overlapping symptoms of other disorder(s) as noted earlier. Therefore, a multifactorial approach is required to make an accurate diagnosis.
The primary method of diagnosing depression is still reliant on techniques such as structured diagnostic interviews, the clinician rating scale interview, and the self-rating scale method based on the symptoms.9
However, newer techniques such as genomics, transcriptomics, proteomics, metabolomics and imaging are now claiming their respective places when it comes to diagnosing depression, although the practical applicability of these techniques is still being appraised in the world of psychiatry.10
Once the diagnostic process is completed, and based on the severity of symptoms and the degree of functional impairment, depression can be classified as mild, moderate or severe, with the mortality and morbidity risk varying accordingly.
Depression and comorbidity
The concept of comorbidity is not new, but in cases of mental health disorders, it is more problematic given that many mental illnesses share similar symptoms.
The lifetime association of depressive disorder with other comorbid psychiatric disorders, such as substance abuse disorder, generalized anxiety disorder and post-traumatic stress disorder, has been found to be significant.11 This can result in complex and sometimes inappropriate diagnostic evaluations potentially causing additional economic burden.
Treatment advances and future trends
Treatment of depression is possible. However, the treatment regimen needs to be individualized because what works for one person may not work for someone else. That is why it is very important that all the relevant factors, along with the possible pros and cons of each treatment, be discussed before a particular approach is adopted.
Any of the regimens outlined below can be utilized to treat depression either in isolation or in combination with one another:
As noted earlier, the severity of depression may vary based on the number of symptoms displayed by the individual, so the treatment will also vary considerably. It is likely that combination therapy would be required for more severe forms of depression.
Physical treatments such as ECT, newer treatment modalities such as transcranial magnetic stimulation (TMS), deep brain stimulation, magneto- convulsive therapy and vagus nerve stimulation might prove promising in the treatment of depression in the near future. With the exception of TMS, which is now being used and accepted widely, the other treatments are still in their initial trials.17
Furthermore, preliminary results of certain innovative techniques such as pharmacological advances (glucocorticoid receptor antagonist, substance P-receptor antagonists and NMDA receptor antagonists) and focal brain stimulations (deep brain stimulation, magnetic seizure therapy, transcranial magnetic stimulation, vagus nerve stimulation) suggest that more effective treatment of depression is possible,18 and, therefore, some groundbreaking technology for the treatment of depression could be on the horizon.
An insurance medicine analysis
Mortality
The association between depression and all-cause mortality has been widely explored, and studies indi- cate that mortality rates are higher among depressed individuals. In a study by Cuijpers, Pim, et al. (2017) it was concluded that mortality is 1.5-fold in depressed individuals when compared with the general population (relative risk (RR) = 1.52 [95%CI, 1.45-1.59]).19
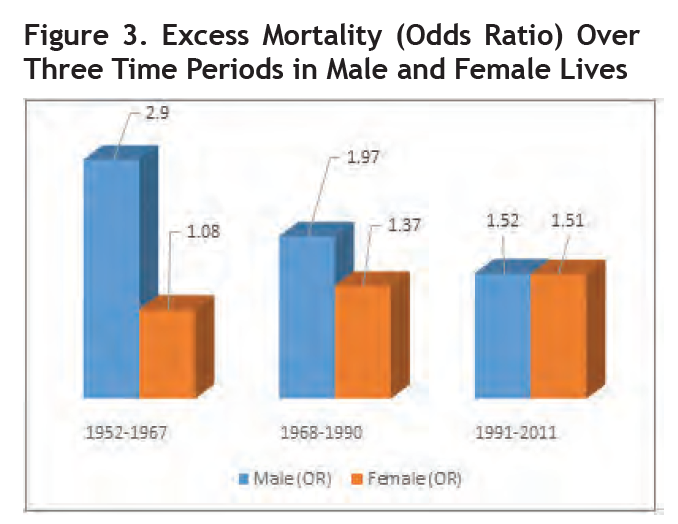
In another study by Gilman and Stephen et al.,20 time trends in mortality for depressed individuals from 1952 to 2011 were captured in three different time periods. They noted that despite advances in treatment over 5 decades, the excess mortality (odds ratio [OR]) in depressed individuals still exists. Of note, the excess mortality in females with depression has been increasing since the 1970s and is now similar to that of males (OR = 1.52, 95%CI 1.09-2.13 for males and OR =1.51, 95% CI 1.11-2.05 in females). Please refer to Figure 3, next page.
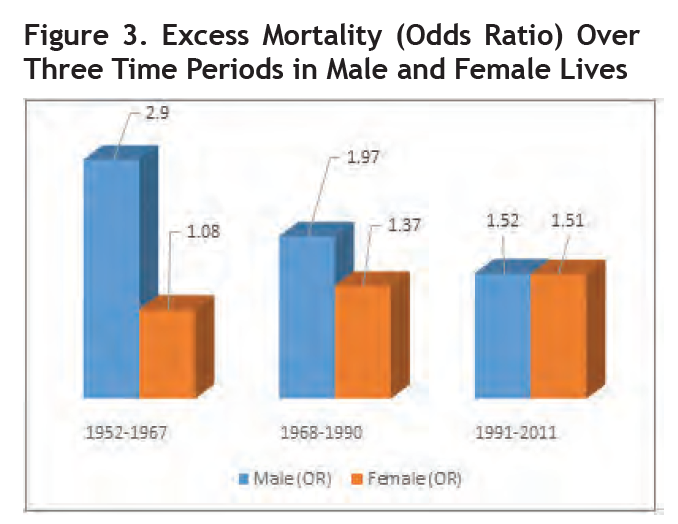
Source: Adapted from Gilman and Stephen et al., "Depression and Mortality in a Longitudinal Study."
Does depression increase the risk of suicide?
Major depressive disorder increases the risk of suicide when compared with individuals who are not depressed. However, the risk of death by suicide will vary in accordance with the severity of the disorder.21
Some possible correlation does exist between suicide and depression according to available evidence:
One in six patients suffering from major depression dies as a result of suicide.22
The lifetime risk of suicide among individuals with untreated depression ranges from 2.2% to 15%.23,24
Depression is present in at least 60% to 70% of all suicides.25
When alcohol or substance abuse is concomitant, the risk of suicide increases significantly.26
Overall, there is a plethora of research which substantiates the impact that depression has on mortality. Therefore, all possible relevant factors should be carefully evaluated at the time of risk assessment.
Morbidity
Depression can significantly hamper the normal functioning of activities of daily living, cause issues with social and personal relationships, and impact chronic physical disorders, all of which can sometimes lead to unstable employment as well. Consequently, this combination of factors can translate into various lifestyle-related diseases and many more physical illnesses such as diabetes, heart disease, chronic pain and fibromyalgia.27
There are numerous studies which have analyzed and concluded a positive correlation between depression and incident risks for the following:
WHO lists depression as one of the leading causes of disability worldwide, with the risk of disability among depressed individuals being close to 50%. This can be higher in individuals with severe forms of depression, especially where there are comorbid anxiety disorders or substance and/or alcohol abuse.33
The greater the severity of the depression, the higher the rate of health care service utilization.34 The World Mental Health survey predicts that by 2030 unipolar major depression will be a leading cause of total disability worldwide.35 This projection will have a significant impact not only on the way health care services will get utilized, but also on the ways the insurance industry (life and health) will have to adapt.
Implication for life insurance and living benefits The continuous evolution of diagnostic tools and treatment modalities means the risk profile of those with depression is gradually improving. However, at the same time, the prevalence is on the rise among young adults.
Studies indicate a higher excess mortality in individuals with depression in comparison with those who are not depressed. Furthermore, suicidal ideation/thoughts are commonly observed in severely depressed individuals, and therefore the mortality risk needs more careful assessment in accordance with the severity.
Despite the risk of increased mortality, individuals with depression should be considered insurable. The proper execution of risk assessment in accordance with severity is vital as in its chronic form, and with moderate-to-severe intensity, depression may become a serious health concern, and at its worst could lead to possible suicidal ideation.
Turning to morbidity, depression can frequently lead to significant disability as a result of the perception of negative social stigma that might prevent an individual from seeking medical care, as well as other, sometimes cumulative effects on a person’s physical health.
The treatment is lengthy in the majority of cases and consists of various permutations and combinations of therapy which can, in some cases, lead to increasing levels of anxiety. Additionally, those suffering from mental health issues may be at higher risk of other chronic disorders, including, but not limited to, diabetes, coronary artery disease and cancer. Thus, when assessing individuals with depression for morbidity or living benefits, it is necessary to be cautious. However, as many will be insurable for cover, careful assessment of each individual is critical.
Summary
Depression is treatable. However, some individuals suffering from depression do not recognize that they are depressed or have trouble asking for help because they are embarrassed and worry about potential social stigmatization.
Here are some key takeaways to focus on while underwriting individuals with depression:
Individuals with depression may be insurable, but the risk will vary in accordance with the severity of the depression.
The greater the severity of the depression, the higher the probability the individual may suffer from comorbid mental or physical health conditions, including alcohol or substance abuse disorder.
The risk of suicidal ideation or attempt is higher among depressed individuals, and depression is frequently present in individuals whose death results from suicide. Again, the severity of the depression along with any co-morbid mental or physical health condition(s) are key factors that necessitate proper attention at the time of risk assessment.
Although mortality appears to be higher among depressed individuals, morbidity remains a significant concern as well. It is important to consider how depression will drive health care utilization in the future and the impact that may have on life and health insurance companies.
In conclusion, along with other relevant factors such as proper diagnosis and adequate treatment, creating more awareness of the disorder is crucial to achieving desirable and sustained outcomes.