Eradicating diseases caused by viral pathogens on a global scale is no easy task. There are only two viruses ever to be eradicated in human history: smallpox (variola virus) and rinderpest virus.
Smallpox was declared eradicated in 1980 while rinderpest, a deadly virus in cattle, was eradicated in 2011. From the introduction of the smallpox vaccine in 1796, it took nearly two centuries to eradicate the disease. It will take a momentous effort by nations around the world to work towards global elimination, and possible eradication of COVID-19, caused by the SARS-CoV-2 virus. Herd immunity can only be achieved when there are enough people with acquired immunity through natural infection or vaccination to stop transmission. One of the biggest challenges in eliminating the SARS-CoV-2 virus is the emergence of significant new variants for which existing vaccines may not fully protect against severe illness and death.1, 2
A pandemic is an epidemic occurring worldwide, or over a very wide area, crossing international boundaries and usually affecting a large number of people. An epidemic is an unexpected increase in the number of disease cases in a specific geographical area. For an epidemic to occur, the reproductive number (R) must be greater than 1, representing a growth in infection rates. The reproductive number is a measure of the potential for the virus to spread through a previously uninfected population. It is calculated by averaging the number of new infections resulting from a single infectious case.3
The original severe acute respiratory syndrome (SARS) pandemic lasted just 18 months and came to an end by early 2004. Like SARS-CoV-2, the virus passed from person to person via respiratory transmission, but the pandemic was brought under control using only public health measures. How? One of the biggest differences between SARS and SARS-CoV-2 is that SARS was mostly transmissible when people displayed obvious signs of infection. Therefore infected individuals could be identified early, isolated, and prevented from creating onward transmission. SARS-CoV-2 however is transmissible before any obvious signs of infection are apparent, or even when it remains asymptomatic, making it more difficult to control. It is probable, based on the factors discussed in this article, that SARS-CoV-2 will become an endemic virus.4
Detailed below are some key reasons why COVID-19 will likely stay with us for months, if not years to come. Insurers should take note of the different factors that make it likely that SARS-CoV-2 will become endemic. These can then be accounted for in future product planning and pricing, underwriting terms, and in setting claims expectations.
But first, a little about viral elimination and eradication
Viral eradication refers to the complete and permanent worldwide reduction to zero new cases of the disease through deliberate efforts. It can only be achieved when there is viral control (i.e. the reduction of disease incidence, prevalence, morbidity, or mortality to a locally acceptable level due to deliberate efforts). However, disease elimination does not require the complete eradication of disease but rather the elimination of disease incidence in a specific geographical area, such as has been achieved with cholera and polio. There are no known cases of viral extinction, where a specific infectious agent no longer exists in nature or in the laboratory. Smallpox is not considered extinct as there are still two official repositories of the smallpox virus, one at the State Research Center of Virology and Biotechnology VECTOR in Russia, and the other at the Centers for Disease Control and Prevention (CDC) repository in Atlanta, Georgia, U.S.A.5,6
Most campaigns to control or eliminate viral disease rely on vaccination strategies that mirror the global approach used to eliminate COVID-19. Although it is possible, if not probable, that SARS-CoV-2 will evolve into a winter seasonal virus like influenza, this may not occur until vaccination rates significantly increase around the world. As of October 5, 2021, 46% of the global population had received a first dose and 34% had received a second dose of a vaccine for SARS-CoV-2.7
What we know about SARS-CoV-2
SARS-CoV-2 is a ribonucleic acid (RNA) virus which means that the genetic material for the virus is encoded in RNA. Deoxyribonucleic acid (DNA) viruses usually replicate in the nucleus, while RNA viruses usually replicate in the cytoplasm of the host cell. Studies have shown that “pandemic-potential” viruses, i.e. respiratory-borne RNA viruses, are more likely to replicate in the cell’s cytoplasm. The Coronaviridae family of viruses, to which SARS-CoV-2 belongs, is known to have a high replication rate compared to other RNA viruses such as Ebola and polio. RNA viruses such as SARS-CoV-2 tend to mutate more frequently than DNA viruses, as they replicate in large numbers daily and make more ‘mistakes’ during viral replication. For example, the D614G variant, one of the first variants of the SARS-CoV-2 virus in the Wuhan reference strain, led to increased transmission rates.8, 9
Persisting viral infections in different geographical regions will mean that SARS-CoV-2 will likely continue as an endemic virus with seasonal peaks. Maintenance of long-term antibody response is critical to protect against severe illness and death from the SARS-CoV-2 virus. Infections may increase in individuals with waning antibody response or because of viral mutations.9
A look at factors influencing viral elimination
- Herd immunity
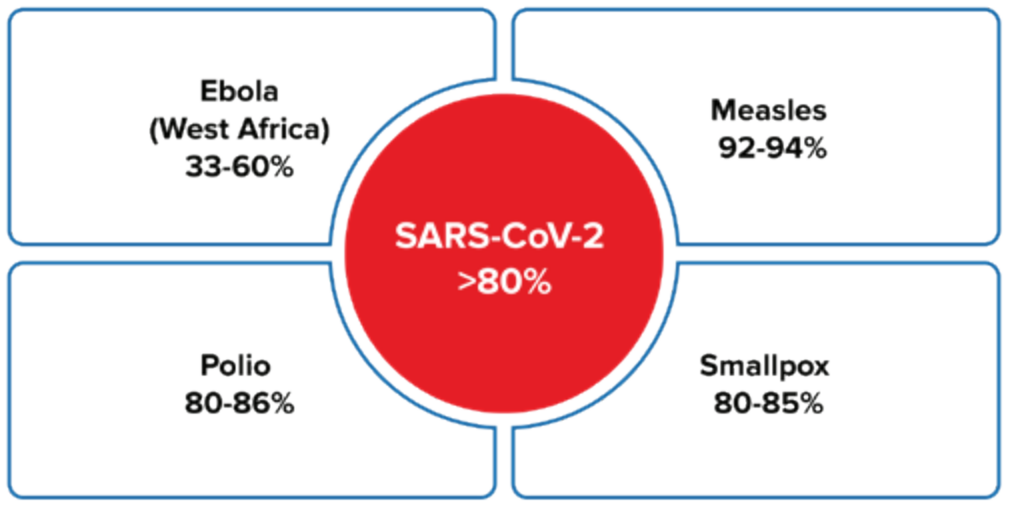
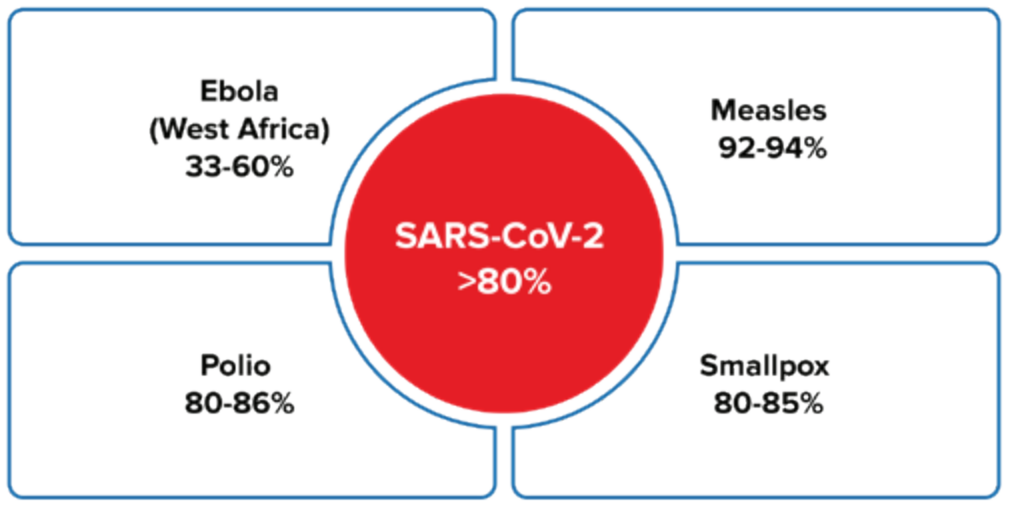
To achieve herd immunity, viruses that transmit much more readily between people require a higher percentage of the population to be immune. Herd immunity may, however, prove temporary if there is an interruption in vaccine supply or if current vaccines become less effective against new variants. The now dominant Delta variant of SARS-CoV-2 is highly transmissible, making it hard to achieve herd immunity. Countries that have a higher proportion of more virulent variants are less likely to achieve herd immunity. It may also be the case that herd immunity is only achieved regionally because of ongoing outbreaks of COVID-19. 9, 10
Figure 1:
Herd immunity threshold (%)3, 11
- Incubation period
The average incubation period for SARS-CoV-2 is 5 days (range 2 to 14 days), which allows for asymptomatic spread of the virus. A recent study showed that SARS-CoV-2 viral load was highest at the time of symptom onset, suggesting that viral shedding has peaked before any symptoms are obvious. This compares to the influenza virus, where the incubation period is only 2 days (range 1-4 days).12 Even the more serious coronaviruses such as SARS and Middle East respiratory syndrome (MERS) did not have as frequent incidence of asymptomatic transmission as SARS-CoV-2.9
- Laboratory testing
Control of asymptomatic infection can only be achieved if there is rapid access to accurate and reliable testing. RNA polymerase chain reaction (PCR) tests are the gold standard for diagnosing SARS-CoV-2. While rapid antigen testing (RAT) is being used widely, it is less sensitive and should only be used early after the onset of symptoms. For diagnosis of SARS-CoV-2, the World Health Organization (WHO) has recommended that a RAT kit needs to meet a minimum performance requirement of at least 80% sensitivity and 97% specificity.13
- Symptomatic disease
Distinct pathogenic symptoms make it easier to control transmission by isolating patients until they have made a full recovery and are no longer infectious. Smallpox caused visible skin sores and blistering, the measles virus presents an obvious body rash, and Ebola virus has symptoms of high fever and unexplained hemorrhaging or bruising. However, only 5% of polio infections result in symptoms, while tuberculosis (TB) often shows no obvious signs of infection; there are an estimated 1.7 billion people globally living with latent TB.2 Up to half of infected individuals with SARS-CoV-2 are asymptomatic but remain infectious and can unknowingly transmit the virus to others.14
- Temperature and climate related factors
Preliminary opinions suggest that temperature and climate-related factors could influence the spread of SARS-CoV-2. At the beginning of the pandemic, countries with the highest number of COVID-19 cases were in the Northern Hemisphere, including China, Iran, Western Europe, and the United States.15 Past studies of the influenza virus have shown that the closer a country is to the equator, the lower the effective reproductive number (R). 3
- Vaccination
Estimates to date indicate that only 4-7% of the global population has been infected meaning that mass vaccination is the most likely way to control infection rates. Years of research meant that pharmaceutical companies were able to rapidly produce an effective vaccine against SARS-CoV-2. The availability and uptake of a vaccine against airborne viruses such as SARS-CoV-2, influenza, and measles greatly reduces rates of transmission.4
- Vaccination hesitancy
There has been much distrust in COVID-19 vaccines based on anti-vaccine misinformation campaigns and a lack of public knowledge regarding the depth of research that supported vaccine development and testing. It is essential for public health authorities to win trust and support for vaccination if communities are to be successful in eradicating disease.
- Viral pathogenicity and virulence
The duration and efficacy of immunity from either natural infection or vaccination depends upon the pathogenicity and virulence of a virus. Pathogenicity is the ability of a virus to cause disease when a host is infected, while virulence refers to the likelihood of the virus causing severe disease in those who are infected. Immunity also depends upon the efficacy of the vaccine and the ability of an individual to mount an immune response against a virus, hence vaccine failure can allow for future transmission of a virus.3
- Viral transmission
Airborne diseases are caused by pathogens transmitted from an infected person via coughing, sneezing, or close personal contact. “Contact” diseases are transmitted when an uninfected person has direct bodily contact with an infected person or has indirect contact with an infected person’s environment. The risk of viral transmission from person-to-person is greater for airborne pathogens; one study published in August 2020 showed that a person in the early stages of SARS-Cov-2 infection emitted millions of viral particles per hour through breathing alone.16
- Viral reservoirs
Viral reservoirs can be harbored by animals (zoonoses) or humans. However, zoonotic reservoirs are more resilient because these viruses can be harbored within animal populations undetected and emerge repeatedly to infect and re-infect human populations. Dengue fever and Zika virus are transmitted to humans from mosquitoes, while SARS and SARS-CoV-2 may have been transmitted from bats to humans. Mosquitoes may present greater risks as vectors of disease because of their wider geographic reach compared to other zoonotic hosts.10
Conclusions
Elimination and eradication of viruses that cause significant morbidity and mortality are the ultimate goals of disease control. Clearly the method and timing of viral transmission, as well as the ability of a virus to frequently mutate are significant factors affecting infection rates. SARS-CoV-2 is unlikely to be eradicated for many years to come, but as vaccination rates increase and viral control is achieved, the burden of disease will shift from managing case counts to managing cases of severe illness and deaths. Insurers are likely to see declarations on application forms of past COVID-19 infection or of long COVID for some time to come, but it is probable that these disclosures will become less frequent each year as nations approach elimination of SARS-CoV-2.
As the pandemic evolves, new evidence and data-driven insights will continue to emerge, which RGA will continue to investigate.