In May 2016, The American Association of Clinical Endocrinologists (AACE), the American College of Endocrinology (ACE), and the Associazione Medici Endocrinologi (AME) issued the latest update of their Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules1.
One of the goals of this update was to stratify the risk represented by different ultrasound images of thyroid nodules. Older guidelines did not have the same emphasis on ultrasound patterns, which underwriters are seeing more frequently in attending physician statements2, 3, 4.
The update includes fine needle aspiration (FNA) recommendations as well as five histologic classifications and comprehensive treatment recommendations. The latter two will not be addressed in this brief report. The new update also addresses both the American and British Thyroid Associations ultrasound thyroid nodule classification schemes.
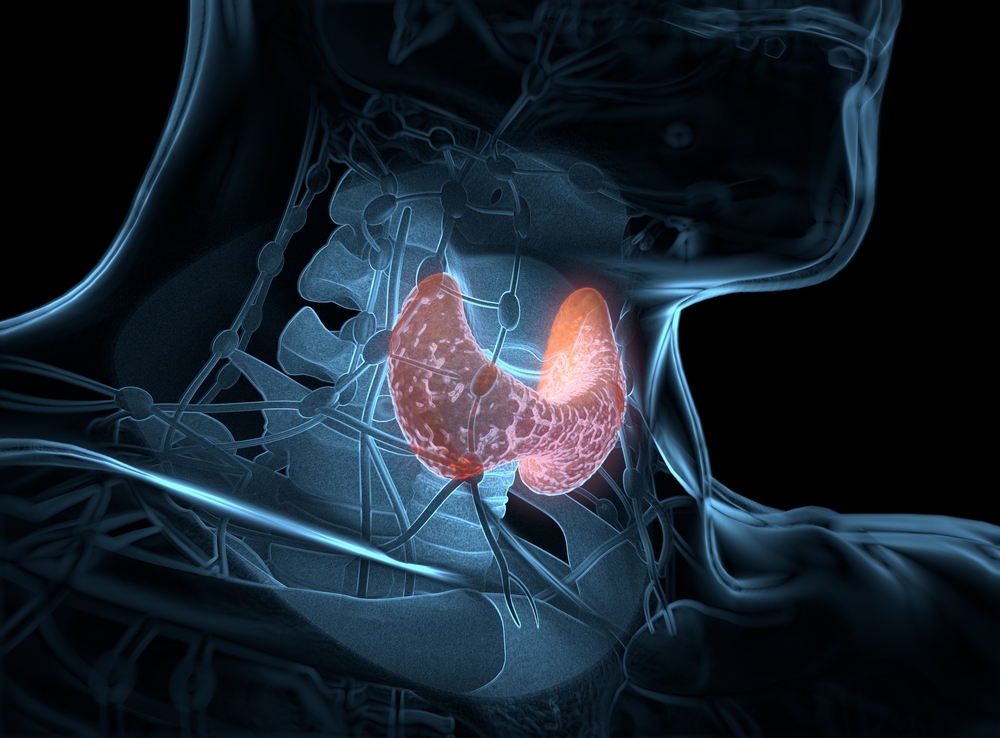
Prevalence of Thyroid Nodules
Large nodules exist in 5% to 8% of the healthy adult population6, 8 whereas small nodules (<10 mm) exist in 50% to 60%1, 5. Only about 2.5% of all thyroid nodules are malignant 6,7.
Patient Characteristics
The presence of any historical or clinical findings can impact the interpretation of the guidelines from the AACE/ACE/AME. Adverse history can include personal or family history of thyroid cancer, multiple endocrine neoplasia (MEN), or personal history of neck irradiation. Clinical findings such as dysphonia, dysphagia, dyspnea, anterior neck pain, nodule enlarging on exam, lymphadenopathy, and presence of hypo- or hyperthyroidism add additional risk consideration 6, 8. Age under 14 years or over 70 also increases malignancy potential, as does being male1.
Guidelines: Malignancy Risk and Recommended FNA Based on Ultrasound Findings 1, 6, 7, 4, 9
Thyroid ultrasound results can be divided into favorable and unfavorable features. As the number of unfavorable features increases, so does the risk of malignancy 1, 6, 9, 10.
These guidelines are for individuals without adverse histories and clinical features described above in “Patient Characteristics” unless otherwise noted.
Any nodule <5 mm should be monitored and should not be biopsied with FNA regardless of the ultrasound characteristics. Even with the adverse features FNA is not recommended if scintigraphy shows normal function.
Patients with multinodular goiter have the same risk stratification guidelines for their nodules as would a patient with a solitary nodule1. For multinodular goiter, each nodule is classified and the nodules with the most adverse features should be biopsied. The guidelines support performing FNA on no more than two nodules1.
Class 1 Lesion: Low-Risk Malignancy - ~1%
- cysts with fluid component >80%
- isoechoic spongiform nodules, either confluent or with regular halo
- FNA if >20 mm and with adverse patient history features present (described on previous page) or enlarging nodule
Class 2 Lesion: Intermediate Risk Malignancy - ~ 5% to 15%
- not a definite benign appearance
- cystic and some solid components
- slightly hypoechoic, isoechoic, or indeterminate hyperechoic spots
- ovoid to round shape
- margins may be smooth or ill-defined
- intranodular vascularization
- continuous calcified rim
- elevated stiffness at elastography
- FNA if >20 mm
Class 3 Lesion: High-Risk Malignancy - ~50% to 90%
Has at least one of the following suspicious features:
- markedly hypoechoic
- spiculated or microlobulated margins
- microcalcifications
- height greater than width
- disruption of a calcified rim
- capsular abutment
- pathologic lymphadenopathy
- FNA if:
- Nodule >10 mm
- extension beyond the hyroid
- pathologic lymph nodes
- vascular features or mass effect on the jugular vein by the lymph nodes
- consider FNA if nodule is 5 mm to 10 mm, depending on clinical setting
Managing Ultrasound Results
The principal goal of a thyroid ultrasound is to find or rule out cancer 1, 8, 5. If a nodule is found, appropriate clinical follow-up must acknowledge the dangers of over-investigation1,11, 12, which can include excess radiation, bleeding, surgical complications, anxiety, anesthesia risk, hospital-acquired infections, and scarring. Surgical complications can include vocal cord paralysis (due to nerve damage), hypothyroidism and hypoparathyroidism7, 11, 12.
Underwriting Considerations
Understanding the natural history of lesions found during thyroid imaging and whether or not they are meaningful to prognosis or represent increased mortality or morbidity risk is essential to underwriting.
Thyroid ultrasound reports are frequently encountered in attending physician statements. It is essential for risk assessors to understand the risk associated with findings even if not clearly stated in the report, and from there determine if appropriate follow-up testing has been scheduled or performed. The historical and clinical features of the proposed insured must also be considered in order to interpret ultrasound findings properly. Taking all of this information into consideration should assist in reaching an appropriate underwriting decision.