Introduction
Sepsis has recently been attracting significant attention from both medical and non-medical communities. The condition is now considered a medical emergency of equal importance with myocardial infarction (MI) and stroke. The early warning signs and symptoms of the latter two are well known to the public and have established emergency treatment protocols. With sepsis, the medical community is strengthening education for the general public about its risks, but work remains to be done. However, there is now a growing consensus among health care professionals that sepsis protocols are beneficial and can provide both life- and cost-saving outcomes.
Somewhat controversially, implementation of sepsis protocols is being mandated by some U.S. states in an attempt to decrease its mortality rate.
Definitions
One of the great difficulties in assessing, diagnosing and treating sepsis has been its ever-changing medical definition. As sepsis’ pathobiology becomes clearer and medical understanding evolves, so too does its definition. Sepsis does not have one etiology and one clinical manifestation: it is a syndrome with varying findings, and no gold standard diagnostic test yet exists.
The many and diverse definitions sepsis has had over the years has made it difficult to track and observe its true epidemiology, thus complicating analysis and comparison of clinical studies on the condition.
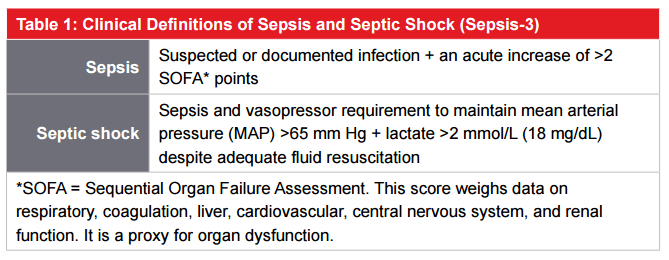
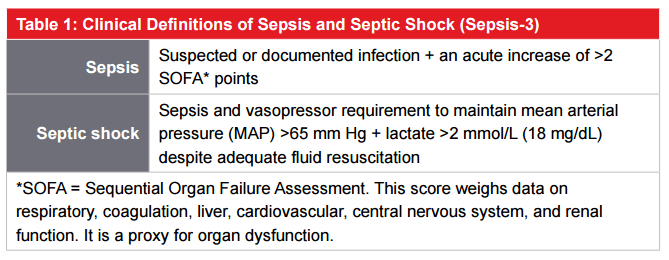
In 2016, the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)2 was released – the first revision of sepsis definitions since 2001. It defines sepsis as “life-threatening organ dysfunction caused by a dysregulated host response to infection,” and septic shock as “a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality.”
The Sepsis-3 clinical definitions are shown in Table 1.
It is hoped that these new definitions will enable better case definition, leading to earlier identification of sepsis, rapid and goal-directed clinical intervention, improved outcomes, and better standardization of epidemiologic and research data.
Incidence Rates
Historically, most incidence studies of sepsis were done using insurance claims data, due to its greater availability. However, due to coding issues and the changing definitions of sepsis over time, the reliability and comparability of past studies is questioned. Additionally challenging is the fact that incidence rates and trends vary between Western and low- and middle-income countries,3 making comparisons more difficult. Nonetheless, most studies would suggest that incidence rates have been increasing for at least 10 years. Speculation of cause include an aging population, increasing use of immunosuppressive therapies, and individuals in general having more comorbid conditions. A recent study, however, which compared clinical and claims data from 2009 through 2014, demonstrated no increased incidence based on clinical data. Claims data, however, suggested a 10% per year increase over that same period. The study’s authors emphasized the importance of using clinical data to establish more accurate incidence trends.4 If incidence rates are truly increasing, health insurers and medical reimbursement policies will clearly be impacted. In addition, since sepsis is one of the costliest medical conditions to treat, given the high likelihood of intensive care unit admissions and prolonged hospital stays, stop-loss portfolios may be increasingly affected as well.
Treatment Protocols
The difficulty in developing treatment protocols for sepsis is the fact that it is not a disease but a syndrome and it presents heterogeneously in patients. In response to the Sepsis-3 guidelines, the Surviving Sepsis Campaign (SSC), a joint collaboration of the Society of Critical Care Medicine and the European Society of Intensive Care Medicine,5 recently updated its sepsis guidelines and treatment protocols. These guidelines, or “bundles,” are standardized sets of interventions which, when implemented as a group, have more favorable impacts on outcomes. The bundles include recommendations for obtaining blood lactate levels and blood cultures, administering broadspectrum antibiotics, and giving intravenous fluids, if indicated, all within three hours of presentation. Additional interventions should be completed within six hours of presentation.
There is also now a movement to legislate the treatment of sepsis. In 2013, the State of New York (U.S.) began mandating that hospitals follow protocols, such as those promoted by the SSC, for the early identification and treatment of sepsis. Data now indicates that completing a bundle in less than three hours can reduce in-hospital mortality. Nonetheless, these regulations remain controversial.6
Mortality Outcomes
Most studies have demonstrated that sepsis’ mortality rate has been decreasing. A report from Australia and New Zealand showed absolute mortality rates from sepsis had decreased from 35% to 18.4% (almost 50% relative risk reduction) from 2000 to 2012.7 Mortality rates from sepsis have also decreased in the U.S., with one meta-analysis showing a decrease from 46.9% in the period 1991-1995 to 29% in the years 2006-2009.
A more recent review of U.S. clinical data demonstrated a decrease in in-hospital mortality due to sepsis by 3.35% per year from 2009 to 2014. There was, however, no change in the rate of death or discharge to hospice. This study therefore challenges other reports supporting a decreasing mortality rate from sepsis.4
Sequelae
According to a 2017 study, sepsis survivors have an exceptionally high 30-day unplanned hospital readmission rate (12.2%) compared with MI (1.2%), heart failure (6.7%), pneumonia (5.2%), and COPD (4.6%), and account overall for 14.5% of readmission costs. These data highlight the importance of discharge planning for survivors of sepsis.9 Another study, from 2014, demonstrated a 17.9% 30-day readmission rate, but also found this increased to almost 50% within one year.10
The cognitive and functional recovery and status of sepsis survivors has also been studied. Among an elderly cohort (mean age 76.9 years), post-sepsis prevalence of moderate to severe cognitive impairment increased 10.6% with an odds ratio of 3.33. This group also experienced functional Activities of Daily Living impairment(s). Importantly, both cognitive and functional limitations persisted for up to eight years. Thus, even though mortality rates from sepsis might be decreasing, survivors can experience permanent impairments. These may impact their ability to live independently or increase other social and medical support needs. These outcomes are certainly relevant to long-term care insurance and potentially to other living benefits products.11
Impact on Insurance and Conclusion
The growing importance of sepsis in the clinical world may have a significant impact on several lines of insurance. The high costs of treatment, both initially and due to high readmission rates, and prolonged hospital stays primarily affect health and stop loss cover. In addition, due to significant sequelae including functional and cognitive impairment, long-term care and other living benefits are subsequently impacted. Insurers would do well to establish a dialogue with all stakeholders in the health care systems of the markets they serve to strengthen early recognition and standardize treatment for sepsis. In doing so, we can create a win-win scenario for both patients and insurers.
References