Mortality experience study using a generalized linear model
Rather than using the traditional actuarial approach, which calculates actual vs. expected (A/E) mortality ratios, we employed a generalized linear model (GLM), a multivariate statistical method. GLM allows for adjustments beyond expected mortality, incorporating variables such as the comorbidity index and interactions between mental health conditions, age, and gender. Another benefit of GLM is the ability to calculate a 95% confidence interval for hazard ratio (HR).
Findings
Prevalence of mental health disorders
Mental health conditions were more prevalent in females than males (Fig 1). However, the gender difference disappeared when considering the most severe cases (Fig 2). There was no age-related difference in either the overall prevalence or severity.
Coexisting higher mortality risk disorders
Individuals with mental health conditions had higher comorbidity scores than those without, suggesting that elevated mortality in mental health patients is influenced by coexisting conditions (Fig 3). This indicates the need for multivariate comorbidity adjustments to isolate the independent mortality impact of mental health conditions
Elevated mortality risk
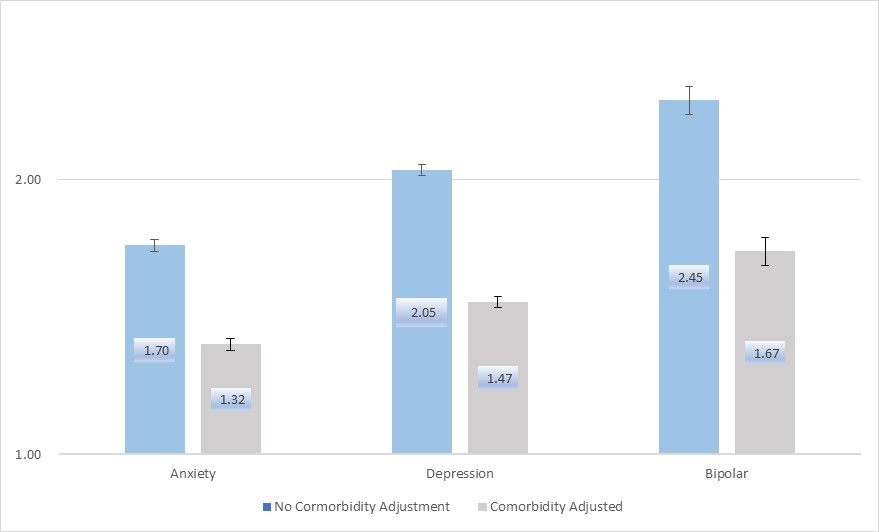
Using the GLM model, all three mental health conditions were associated with higher mortality risks, expressed as hazard ratios (HR). A HR greater than 1 indicates an increased mortality risk, and non-overlapping 95% confidence intervals with 1 confirm statistical significance. After adjusting for comorbidities, the hazard ratios were reduced but remained significant (Fig 4).
Please note that the hazard ratios are meant to illustrate the impact of mental health conditions on mortality. They should not be directly translated into underwriting ratings, as mental health conditions in life insurance underwriting are defined clinically rather than by ICD codes. Additionally, significant differences exist between the insurance population and the general population that are not addressed in this study.
Severity and mortality risk
Mortality risk increased with the severity of each mental health condition, although the severity definitions in the study, based on ICD-10 codes, lacked clinical granularity (Fig 5).
Stronger impact at younger ages
Subgroup analysis revealed that mental health conditions had a stronger mortality impact on younger individuals, with the effect being statistically significant. Mortality risk was slightly higher in males than females, though not all results reached statistical significance.
Conclusions
The primary strength of this study is its large sample size, with over 100,000 recorded deaths, allowing for high sensitivity in detecting associations between mental health conditions and mortality in the general population, even when broken down by age and gender.
However, the study has two key limitations: (1) The classification of mental health condition severity lacks clinical precision and does not correspond to actual clinical severity assessments. As such, the findings on severity and mortality in Figure 5 indicate a positive association in direction but should not be interpreted as quantifying mortality risk based on clinically defined severity. (2) The co-morbidity index is not specific to particular conditions, limiting its ability to assess interactions between mental health and individual co-morbidities.
This mortality study is part of RGA’s comprehensive review of mental health disease risk. The empirical evidence from this study, along with findings from medical literature and RGA’s underwriting expertise, helps shape RGA’s underwriting philosophy and guidelines on mental health risk.
Fig 1. Prevalence of Three Mental Health Conditions by Gender
Fig 2. Prevalence of Severe Mental Health Conditions by Gender
Fig 3. Higher Comorbidity Score Among Individual with Mental Health Conditions than Those Without
Fig 4. Hazard Ratios (95% Confidence Interval) of Three Mental Health Conditions in GLLM Model, With & Without Comorbidity Adjustment
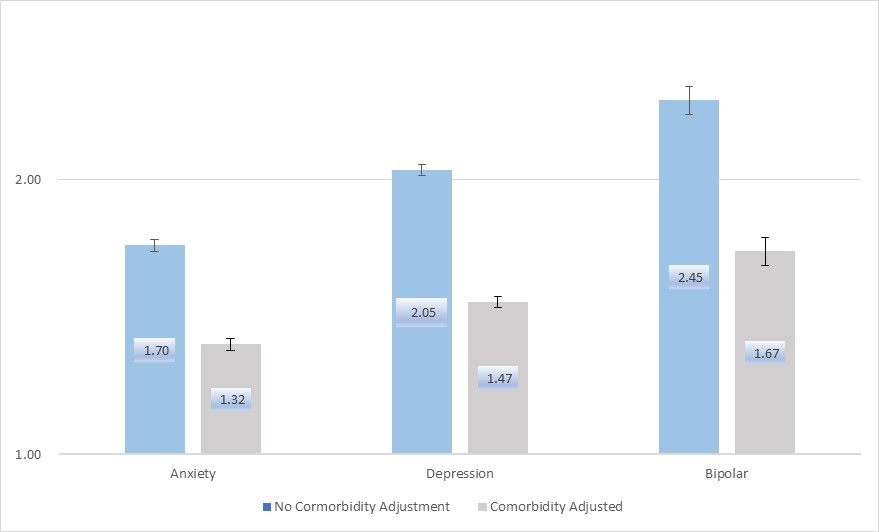
Fig 5. Hazard Ratios by Severity
Fig 6. Hazard Ratios by Age and Sex of the Three Conditions