Significant developments in the field of medical diagnostics during the last decade, such as liquid biopsies, genetic testing, and microbiomics, show growing potential for wider implementation, particularly in the diagnosis of cancer.
Analysis of the microbiome to prevent, diagnose, treat, and even cure disease is likely to impact mortality and morbidity in the future and presents a range of opportunities and challenges to the life insurance industry.
The microbiota is the collective group of microbes that inhabit various sites of the body, while the microbiome encompasses all microorganisms and their genes.
New research continues to emerge on how the human body functions on a microbial level and its impact on health. For example, we now know that Helicobacter pylori infection is linked with an increased risk of gastroesophageal cancer and that human papillomavirus infection is linked with an increased risk of cervical cancer.[1] Roughly 15-20% of cancers are attributable to microbial infections, which may cause inflammation, DNA damage, and cell proliferation.[2] Clearly, microbiomics is an area worthy of further investigation.
What are Microbiomics and the Microbiome?
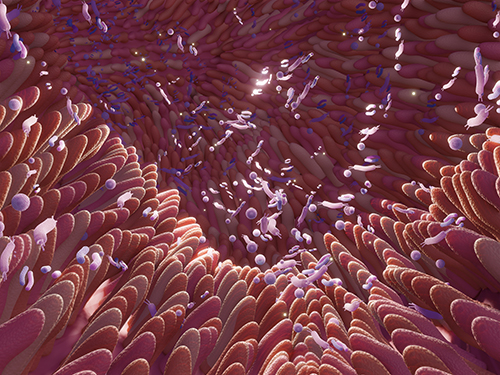
Microbiomics is the study of the structure, function, and dynamics of the microbiome. The human microbiota is defined as the group of microbes that inhabit various sites of the human body and its ecosystem. This microbial ecosystem encompasses all microorganisms (and their genes) that live within and upon us and affect human health and disease, including bacteria, fungi, protozoa, and viruses that live predominantly in the oral cavity, nasal passages, and the gut.[3] Most microbes in the human body are commensal bacteria.
Every human has a unique mix of microbiota called the microbiome. Most of the 39 trillion microbes are found in the gut and include approximately 1,000 different species, while the oral microbiome is the second largest, hosting about 700 different species.[2, 4] The majority of these microorganisms are harmless and involved in regular processes such as digestion of nutrients, the production of vitamins, and immune protection against harmful bacteria.[5]
The microbiome varies significantly from person to person and changes over time as it is influenced by genetics, environment, disease, lifestyle, and diet.[6] Smoking, alcohol consumption, high body mass index (BMI), and exposure to air pollution – all known risk factors for cancer – can alter the microbiome, as can pharmaceuticals and infections. At least 15 different types of bacteria have been found in cigarettes, for example, with smoking leading to dysbiosis (see below) of the oral microbiome.
It is the composition of the microbiome rather than the presence or absence of specific pathogens that may help identify disease development.[7] Disturbances in the microbiome, referred to as dysbiosis, play a role in several conditions such as cancer, cardiovascular disease, irritable bowel disease, and non-insulin dependent diabetes.[8] Specifically, oral dysbiosis has been linked to periodontal disease and cancers of the mouth, esophagus, liver, stomach, breast, lung, colon, and rectum.[4]
The Microbiome and Cancer
Dysbiosis of the microbiome has been associated with the development of cancer.
Much microbiome research is currently aimed at the early detection of lung, liver, pancreatic, and ovarian cancers. These cancers are typically hard to detect at early stages, and hence five-year survival rates are generally very low. As an example, overall survival rates for pancreatic ductal adenocarcinoma (PDAC) are as low as 9% with a five-year survival rate of 11-25%. There is still no effective screening tool for pancreatic cancer, meaning that 80-90% of patients with PDAC present with advanced disease for which there is no viable treatment.[4] Differences in oral, gut, pancreatic, and blood microbiota composition have been identified between PDAC individuals and healthy controls, and microbiome signatures have been identified for triple negative breast cancer and oropharyngeal squamous cell carcinoma.[9] Hence, using microbiomic markers to identify individuals at risk of or with early-stage cancer could transform cancer screening.
Using the Microbiome as a Diagnostic Test
Biological samples of blood, plasma, serum, saliva, urine, tissue, or fecal matter can be collected from an individual and used to assess the pathogenic makeup of the microbiome. Microbes are found not only in healthy human tissue but also in cancer tissues and blood. While using blood plasma or serum is the most widely used biological sampling method, urine provides the greatest source for biomarkers of disease and, unlike blood samples, can be obtained non-invasively.[10]
Microorganisms in the gut can be examined using a stool sample to provide an indication of the type and levels of pathogens in the gastrointestinal tract. However, the number and type of bacteria present can change from sample to sample for the same individual, and only the bacteria’s presence can be determined, not whether the bacteria are alive or dead.[8] One of the main problems in using the microbiome as a marker of disease is the lack of standard references in microbiome diagnostics. Although several commercial microbiome tests are available in the U.S., costing between $250-300, none of them is approved by the Food and Drug Administration (FDA).[6]
Analysis of the overall composition of circulating microbiota could lead to the use of the microbiome as a biomarker for the presence of cancer and the likely prognosis of that cancer. Research shows that ovarian cancers have a distinct composition of viral, bacterial, fungal, and parasitic pathogens, while breast, head, and neck cancers have their own unique signatures. These distinct microbiomes could enable scientists to develop targeted therapies aimed at treating cancers with poor survival rates.[9]
Using The Cancer Genome Atlas (TCGA) studies that identified unique microbial signatures in tissue and blood for most major cancer types, researchers showed that these microbial signatures were predictive when applied to stage Ia-IIc cancer patients. They proved that the plasma-derived, cell-free microbial nucleic acids could discriminate between healthy controls and multiple cancer types, including prostate, lung, and melanoma. These types of studies offer great hope for the development of new cancer-based diagnostics and treatments.[11]
Table
Microbes Associated with Cancer Types
Therapeutics
Dietary modifications may be one way to change the existing microbiome to improve gut health. Rapidly fermentable elements in processed foods may induce excessive bacteria growth in the small intestine, resulting in an unhealthy microbial composition that may induce cancer growth. Conversely, a Mediterranean diet may improve the health of the gut microbiome and provide protection against colorectal cancer.[14] Nutritional strategies may therefore be important in promoting a healthy microbiome.
The microbiome may help explain why some cancer patients respond to checkpoint inhibitors or experience chemotoxicity while some do not. Gammaproteobacteria has been identified as responsible for resistance to chemotherapy used in the treatment of colon cancer.[5] Intratumor injections using engineered bacteria or transplanted bacteria from a healthy donor to alter the microbiome in cancer patients is one method under investigation to combat such resistance.[1] However, using microbes to treat cancer is not new; Mycobacterium bovis has been used to treat bladder cancer, while other microbial products have been used to induce immune activation and tumor regression.[2] Recently, FDA committee advisers approved fecal microbiota transplant therapy for Clostridioides difficile (C. difficile) infection. This investigational therapy involves transplanting beneficial bacteria into the gut of a patient with recurrent C. difficile and has been found to be effective in individuals who failed to respond to first-line antibiotics. Although the FDA does not have to follow the advice of the committee, it frequently does.[15]
Summary
Using the microbiome as a disease screening tool is a promising development and is showing great potential for use in cancer diagnostics and prognostics. Novel diagnostic tools that harness the gut microbiome could lead to earlier identification and treatment of cancers with poor overall survival rates. Identifying microbiota compositions in the presence of disease could help develop new precision treatments and allow healthy individuals to take prophylactic measures against developing cancer. As research moves closer to harnessing microbiome information to improve health outcomes, it opens the potential to improve mortality and morbidity rates, particularly for gastrointestinal tract cancers and those with poor survival outcomes.