Key takeaways
- Any amount of exercise lowered all-cause mortality risk for both the non-obese and obese populations, although mortality benefits were slightly lower for the obese population.
- Generally, meeting or exceeding the recommended ranges of exercise exhibited added mortality benefit compared to less or no exercise for the obese population.
- Higher-intensity, vigorous exercise had additional mortality reduction beyond that of moderate exercise for the obese population.
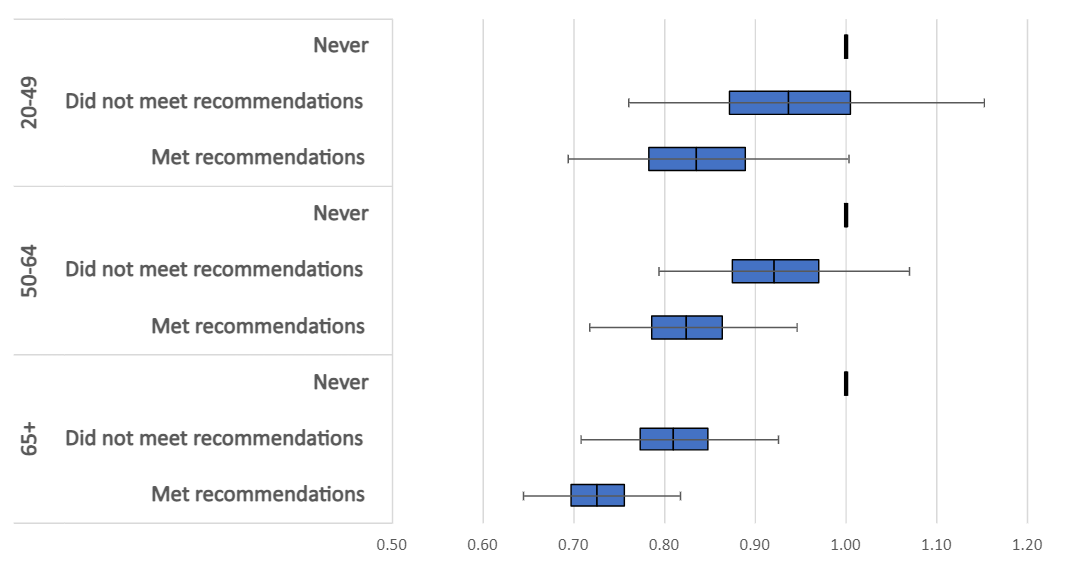
- Obese adults aged 65+ experienced a greater reduction in all-cause mortality from exercise compared to the reduction experienced by younger age groups; however, all age groups generally experienced mortality benefits from exercise.
Amid today’s GLP-1 drug revolution, a new RGA analysis of US health data reveals that good old-fashioned exercise – in nearly any amount – provides a significant reduction in mortality for obese individuals.
These findings are especially relevant for insurers offering or seeking to implement wellness programs geared toward increasing activity levels and promoting healthy lifestyles.
Background
Obesity rates have been steadily increasing in the US for many years. From 2017 to early 2020, approximately 41.9% of US adults 20 and over were considered obese – up from 30.5% in 1999-2000. At the same time, the prevalence of severe obesity – defined as a BMI of 40 or higher – also increased from 4.7% to 9.2% [1].
These trends in increasing obesity carry mortality implications. Obesity is linked to high blood pressure, Type 2 diabetes, many types of cancer, and premature death [2]. Obesity has been classified as the #4 leading risk factor in the US, falling just behind smoking [3].
Figure 1. Deaths by risk factor in the United States, 20211
Recreation of chart from Our World in Data, utilizing data from IHME, Global Burden of Disease (2024) – with minor processing by Our World in Data.
These obesity trends and the corresponding mortality implications present a cause for concern, especially if they persist into the future.
Mortality Analysis
RGA analyzed data from the National Health Interview Survey (NHIS), a US-based survey dataset, with mortality linkage from the period 1987-2015 [4] and developed multivariate survival models to assess the impact of lifestyle behaviors on mortality within the US population, controlling for age, sex, smoking, disease history, health status, and income. These were adjusted based on income and insurable interest to make findings more applicable to an insured population. RGA researchers first categorized the NHIS dataset into obese and non-obese populations, where the obese population was defined as individuals with a BMI of 30 or more, and the non-obese population consisted of individuals with a known BMI less than 30. All-cause mortality experience was broken out by self-reported activity level.
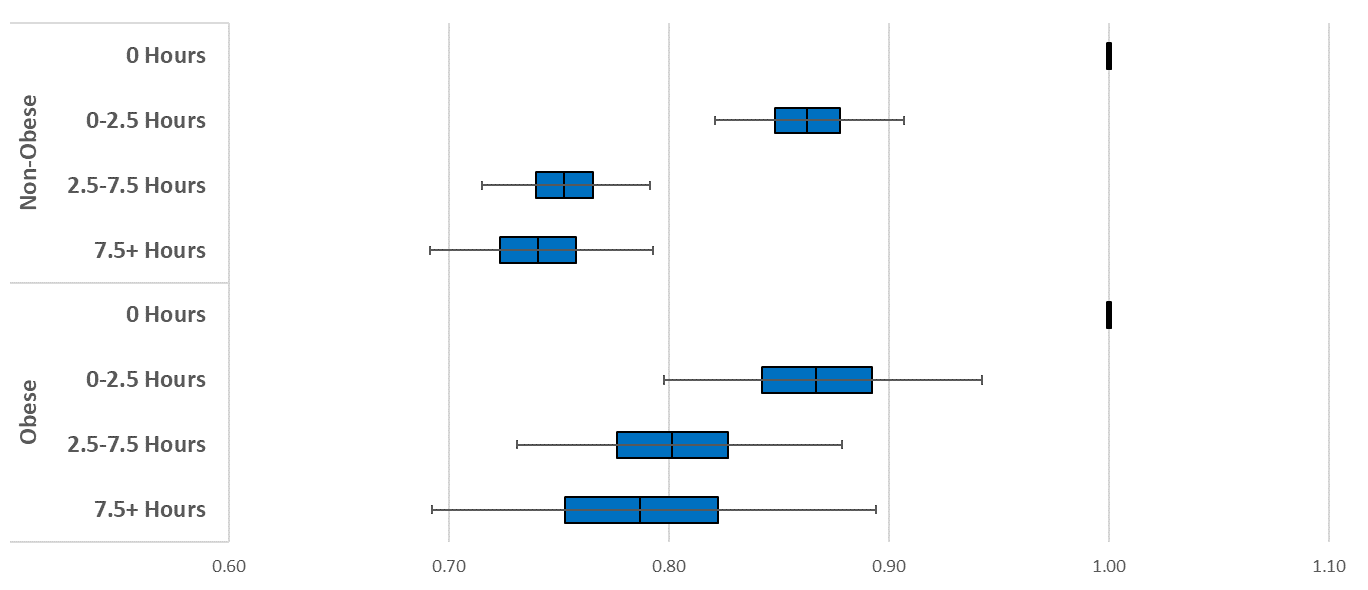
In Figure 2, it is apparent that any level of exercise provides mortality benefits. These benefits appear to be slightly lower for the obese population, but there is still a benefit, nonetheless. More exercise generally improves all-cause mortality risk for both populations, demonstrating that incorporating exercise into daily life is shown to lower mortality regardless of BMI.
Figure 2. All-cause mortality hazard ratios by total weekly exercise duration, excluding those unable to exercise
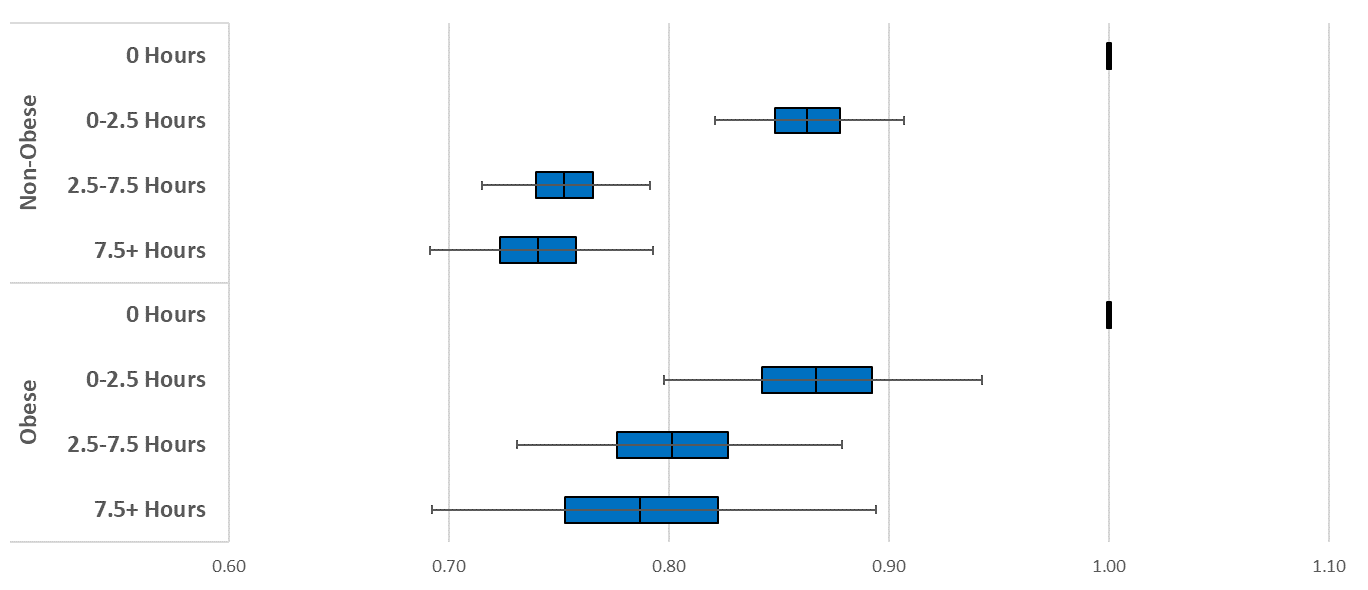
Source: RGA analysis of NHIS data, 1987-2015; multivariate model adjusts for age, sex, smoking, disease history, health status and income.
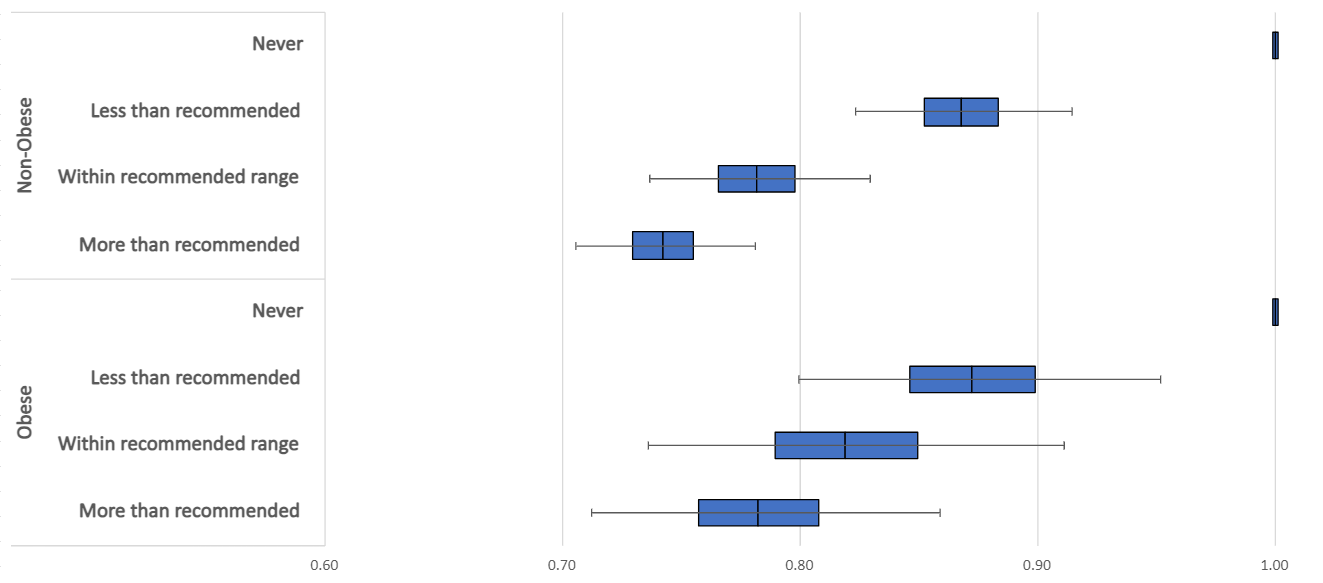
These two populations were then split into activity level groups based on the World Health Organization’s (WHO) recommended ranges of exercise. These recommended ranges not only accounted for the total time of exercise but also were adjusted for intensity of exercise, defined as one of the following:
- 150-300 minutes per week of moderate intensity exercise,
- 75-150 minutes per week of vigorous intensity exercise, or
- An equivalent combination of the above ranges [5].
Results in Figure 3 align well with the results in Figure 2, further emphasizing that increased exercise is generally beneficial for the all-cause mortality of both the obese and non-obese populations, albeit slightly lower effects for the obese population. Both populations may see additional benefit by exercising above the recommended ranges prescribed by WHO.
These results also align well with a study published by the American Heart Association, which indicated that reduced mortality was seen for individuals who exercised two to four times the recommended range[6].
Figure 3. All-cause mortality hazard ratios by the WHO recommended range, excluding those unable to exercise
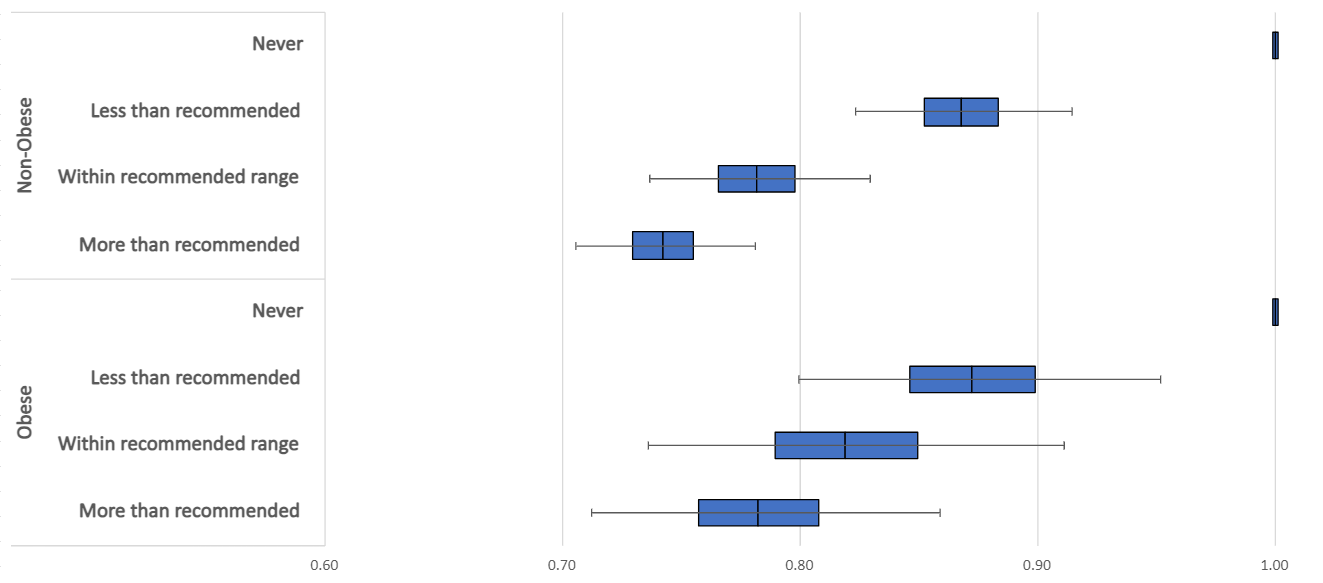
Source: RGA analysis of NHIS data, 1987-2015; multivariate model adjusts for age, sex, smoking, disease history, health status and income.
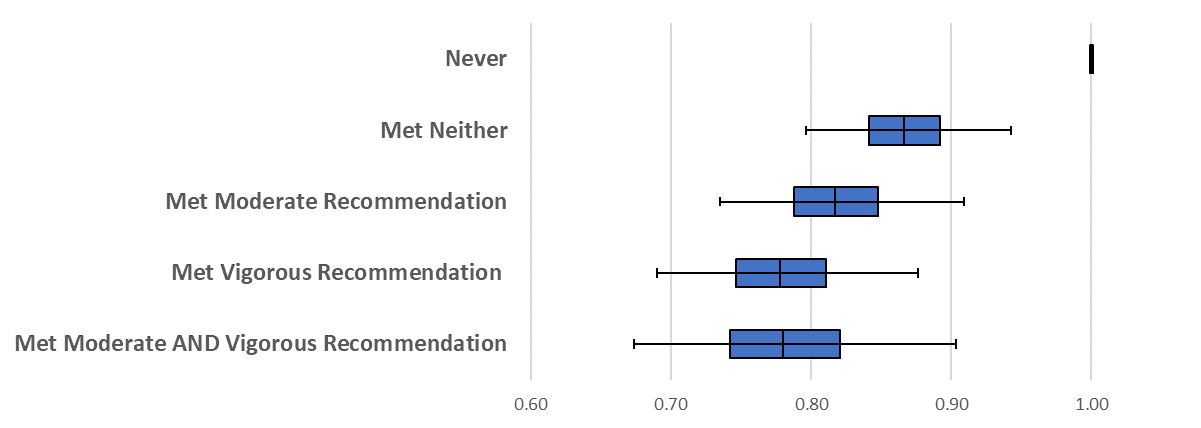
To better understand the impact of exercise intensity, the obese population was further split into different activity groups. Individuals were grouped based on whether they met only the moderate or the vigorous recommendation of exercise, if they met both recommendations, if they exercise but did not meet either recommendation2, or if they chose not to exercise at all.