Cardiovascular disease (CVD) remains the single largest cause of death globally. According to the World Health Organization (WHO), 31% of all deaths cumulatively can be attributed to CVDs, with myocardial infarction (MI) and stroke accounting for 85% of these deaths.1
The estimated cost of managing CVD is expected to rise to $1,044 billion by the year 2030.2 It is thus imperative for insurers to stay current with any updates to the definition of MI, especially, and its consequent impact on claims, underwriting, and product development.
The Fourth Definition of Myocardial Infarction, the most recent update of this important definition, was published in 2018 by a task force consisting of the Joint European Society of Cardiology (ESC), the American College of Cardiology (ACC), the American Heart Association (AHA), and the World Heart Federation (WHF). This article outlines the key aspects of this revision and its potential implications for the life insurance industry, including underwriting guidelines and claims management.
The Evolution of Myocardial Infarction: Understanding and Definitions
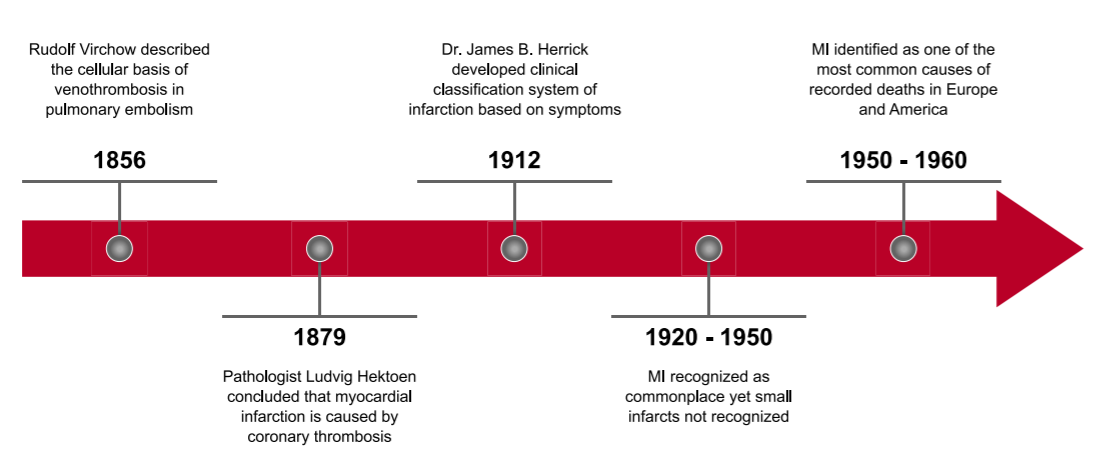
The formal definition of myocardial infarction (MI) can be traced back more than 150 years. The timeline in Figure 1 shows the definition’s evolution and history, from Rudolf Virchow’s description of the cellular basis of venothrombosis in pulmonary embolism, through the 1950s and 1960s – the point at which it was recognized as one of the most common causes of death across Europe and in the Americas.3
The MI Definition’s Post-1950 Transformation
From the late 1950s to the beginning of the 21st century, the World Health Organization (WHO) has recommended several updates to the definition of MI, resulting in different versions. Initially, definitional language was guided by electrocardiographic-based definitions along with specific symptomatic criteria. However, the discovery in the 1980s of the non-enzyme, cardiac-specific biomarkers known as troponins changed MI’s diagnostic criteria completely. By the end of that decade, because of their sensitivity and specificity, the biomarkers troponin T and troponin I had replaced creatine kinase (CK) and creatine kinase-MB (CK-MB) as the preferred biochemical markers for MI, with rises above their normal ranges becoming central to a diagnosis.
Origins of Collaborative and Universal Definitions
In 1971, WHO published a report that established MI as a diagnosis if two of the following three criteria were met:4, 5
- Clinical symptoms
- Definite ECG changes
- Increases in cardiac enzymes CK and CK-MB
One of the first collaborative MI definitions was issued in the year 2000, when the European Society of Cardiology (ESC) and the American College of Cardiology (ACC) came together to craft a clinical and biochemical approach of defining MI.
It was not until 2007, however, that the Global MI Task Force (endorsed by the ESC, the ACC, and WHO) introduced what is today known as the modern method of MI classification, better known as Universal Definition of MI.5, 6
The 2007 definition’s guidelines for diagnosis of MI described the various clinical scenarios in which MI might be diagnosed. The basic notion that myocardial infarction represented myocardial cell death as a result of disruption of blood supply to the heart did not change over time. Five different types of MI, listed in Table 1, were recognized and defined on pathophysiological grounds.
Fourth Universal Definition: Focus on Myocardial Injury
The latest definition of myocardial infarction emphasizes the concept of myocardial injury detected by biomarkers and the importance of defining myocardial infarction only when injury has occurred as a consequence of ischemia. Increasing marker sensitivity for injury has reduced the specificity for infarction and makes it crucial that the clinical circumstances be analyzed in detail.
Acute myocardial infarction is defined as myocardial injury detected by “a rise and/or fall of cardiac troponin with at least one value above the 99th percentile upper reference limit (URL)” which occurs in the setting of acute myocardial ischemia.
It is important to know that myocardial injury can also be a diagnostic entity for other conditions as well. Non-ischemic myocardial injury, for example, may result from other cardiac conditions such as myocarditis or cardiomyopathy, and elevated biomarkers may be found in non-cardiac conditions such as renal failure.7
Essentially the revision of MI definitions not only has an effect on the traditional clinical definitions for the various types of MI but also a secondary effect on other associated cardiovascular disorders such as MI with non-obstructive coronary arteries (MINOCA) and Takotsubo syndrome.
MI Definitions and Subtypes: Comparing Key Differentiators
The detailed evidence used in the latest definition to define the different types of MI remain similar to those in preceding definitions.7 Table 1 (below) provides a general overview.
Table 1:
Types of Myocardial Infarction
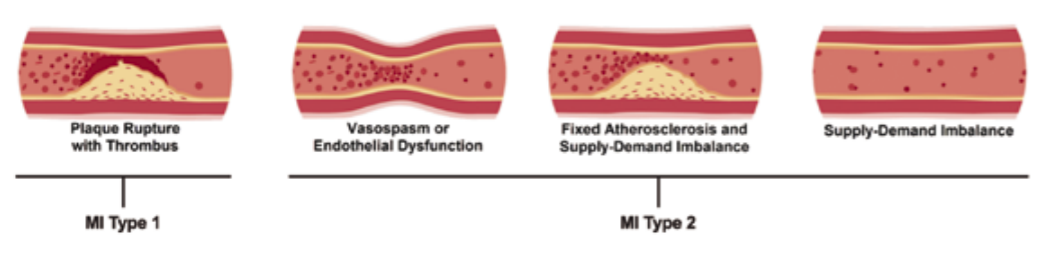
Type 1 | Classical MI. Acute atherothrombosis, caused by coronary artery disease (CAD) with plaque rupture and thrombus formation. |
Type 2 | Caused by a rising imbalance between myocardial oxygen supply and demand in absence of coronary plaque rupture with thrombosis. Type 2 infarction may occur in the context of normal coronary arteries. Varying degrees of obstructive coronary artery disease may accompany this entity and contribute to the supply and demand imbalance. |
Type 3 | Denotes patients suffering from cardiac death before evidence of cardiac biomarker elevation could be made available and with presumed newfound ECG changes. |
Type 4 and Type 5 | These are infarctions arising as a consequence of coronary procedures such as percutaneous coronary intervention (PCI) (Type 4) and coronary artery bypass grafting (CABG) (Type 5). Type 4a infarction is diagnosed if an infarct is caused during the routine deployment of a stent for a coronary occlusion. Type 4b infarction is diagnosed when a previously deployed coronary stent acutely thromboses with the abrupt cessation of blood flow. Type 5 infarction is defined if a myocardial infarction occurs during surgical coronary artery bypass grafting. |
It is often difficult to differentiate Type 1 from Type 2 MI (Figure 2). A diagnosis of Type 1 MI may be made upon the identification of a coronary thrombosis and a ruptured plaque by angiography including intracoronary imaging. A diagnosis of Type 2 infarction requires evidence of an imbalance between myocardial oxygen supply and demand which is unrelated to coronary thrombosis even if an angiogram happens to demonstrate coronary disease.
The Curious Case of Biomarkers: Cardiac Troponins
Troponin is the biomarker of choice for the detection of any form of cardiac injury. Cardiac-specific troponins troponin I (cTnI) and troponin T (cTnT) are known to be highly sensitive markers for the evaluation and diagnosis of myocardial injury and subsequent MI.
The troponin complex in heart muscle cells comprises three specific sub-units (troponin I, T and C). Troponin I and troponin T are considered cardio-specific while troponin C occurs in other muscle tissue.8
The 99th percentile, which has been defined as the cutoff value for troponin elevations for diagnosing MI, is quoted by the various assay manufacturers for all assays. Some laboratories may report age- or gender-specific troponin reference ranges.9
While an MI can only be diagnosed on biomarker grounds when a level exceeds the 99th percentile for a reference population, there is also a requirement that the level be in flux. A rise and/or fall must be identified to avoid false diagnoses in those with medical conditions associated with chronically elevated troponins. The magnitude of change that reflects a true rise or fall depends on assay characteristics, but is usually defined as a change of 20% to 50%.
Type 4a and Type 5 myocardial infarctions require specific orders of magnitude of troponin above the 99th percentile to be exceeded.
If cTn data is unavailable, the cardiac enzyme CK-MB serves as the best alternative marker.
Although there is no question as to the importance of cardiac troponins in the diagnosis of MI, there are a few points to ponder which do not yet have firm conclusions:7
- There is no absolute consensus about the specific criteria to define the 99th percentile URL.
- Although age-dependent assays are not currently mandated or recommended, variability of assay results for individuals age 60+ years or with comorbidities cannot be ruled out.
- The use of gender-specific 99th percentiles is not currently mandated but should be used if provided. Lower values are observed in women compared to men.
Despite the very high sensitivity of the troponin assays already in use, it is possible that even more sensitive assays might be developed to detect myocardial injury, which would likely result in increased MI incidence rates. MI incidence rates could also be affected by assay sensitivity for myocardial necrosis, which may be indicative of false positive MI diagnoses. As the latest high-sensitivity assays are able to detect very small levels of troponin elevation, it is no longer possible to directly equate detectable troponin rises with MI.
Interpretation of an elevated troponin level requires careful consideration of the clinical context. The increased sensitivity for the detection of an elevated troponin will be associated with some loss of specificity for MI since myocardial cell death can occur in many situations other than ischemic infarction.
Understanding Non-MI Troponin Elevations
In cases where troponin elevation occurs without clear associations, such as ECG changes and/or imaging or angiographic findings of acute myocardial ischemia, it could be a result of myocardial injury due to causes other than MI, and could be of cardiac or systemic origin (Figure 3).
Another familiar and common but misleading assumption is that rising and falling troponin patterns only occur in the context of MI. That too needs to be substantiated in context with all other findings as described under the Fourth Universal Definition to confirm MI.7
It is important to understand that the current definition utilizes the terminology “myocardial injury without infarction” from a pathophysiological perspective.
However, it may not be that straightforward from a clinical point of view. Clinicians need to evaluate all possibilities before concluding whether a troponin elevation is due to MI or non-MI conditions.
Imaging Techniques and Diagnostic Testing
Five types of imaging tests are the tests of choice to diagnose MI and related CVDs: echocardiography, radionuclide imaging, single photo emission computed tomography (SPECT), cardiac magnetic resonance imaging (CMRI), and computed tomographic coronary angiography (CTCA).
While echocardiography would help to differentiate non- coronary pathologies known to cause chest pain (e.g., hypertrophic cardiomyopathy), CMRI can help distinguish acute from chronic myocardial injury. CTCA may be used to diagnose coronary artery disease (CAD) in patients with acute coronary syndrome (ACS), and it can also be helpful for acute MI detection.7
Figure 3:
Myocardial Injury for MI- and Non-MI-Related Factors
Reasons for Elevation of Cardiac Troponin Values Due to Myocardial Injury |
Myocardial injury related to acute myocardial ischemia |
Atherosclerotic plaque disruption with thrombosis |
Myocardial injury related to acute myocardial ischemia because of oxygen supply/imbalance |
Reduced myocardial perfusion; e.g.:
- Coronary artery spasm, microvascular dysfunction
- Coronary embolism
- Coronary artery dissection
- Sustained bradyarrhythmia
- Hypotension or shock
- Respiratory failure
- Severe anemia
Increased myocardial oxygen demand; e.g.:
- Sustained tachyarrythmia
- Severe hypertension with/without left ventricular hypertrophy
|
Other causes of myocardial injury |
Cardiac conditions; e.g.:
Systemic conditions; e.g.:
Sepsis Chronic kidney disease Stroke, subarachnoid hemorrhage Pulmonary embolism, pulmonary hypertension Infiltrative diseases; e.g., amyloidosis, sarcoidosis Chemotherapeutic agents Critically ill patients Strenuous exercise
|
Source: Adapted from Thygesen K, et al. Fourth universal definition of myocardial infarction. 2018.
The Insurance Paradox
The evolution of the MI definition over the years has been intriguing. With CVD accounting for 31% of deaths globally and MI being one its chief components, these impairments pose a great challenge to the insurance industry. The impact on various critical illness and cardiac-specific products, as well as on the management of definitions for the covered/exempt conditions defined within each, is most profound.
What are the implications of this latest revision for the insurance industry?
MI Definitions and Subtypes
“Myocardial injury” and its related concepts must be correctly understood, as it is an integral part of the approved definition of MI.
Type 1 MI: Fundamentally unchanged from its previous definitions. The only aspects of the definition that may need standardizing are the associated evidence items needed to confirm it.
Type 2 MI: Type 2 represents one of the pivotal and most challenging talking points of the current updated definition. That acute atherothrombotic plaque is not a prerequisite and instead a sustained tachyarrhythmia with clinical manifestation of MI that could lead to myocardial injury and consequently to Type 2 MI remains a bit of an enigma. The thin line between cardiac injury and infarction may appear to be blurred in patients who are unstable, unconscious, hypoxic, or are mechanically ventilated in the ICU. Furthermore, establishing Type 2 MI is a challenge in itself, given that the rise and fall of troponin values resembles those of other CVDs.
Going forward, Type 2 MI might be seen more frequently as a claimed event under MI. Thus it is important that pricing, underwriting, and claims have a uniform understanding of it and work in cohesion to build guidelines around it.
Type 3 MI: This type of MI has not historically proven to be of significant challenge to the insurance industry as standard CI definitions require a survival period.
Types 4 and 5 MI: Myocardial injury due to coronary procedures is different from ischemia and more prevalent than generally believed. Nearly 32% of patients have procedural myocardial injury after PCI or coronary artery bypass grafting (CABG), but this injury is not necessarily definable as MI.7 The arbitrary order of magnitude of troponin elevation that has been proposed for the purposes of defining procedural MI has limited this as a diagnosis.
The concept of procedural myocardial injury as opposed to procedural infarction must be distinguished for and priced accordingly. Insurance- or product-specific definitions need to recognize this aspect and specify their inclusion or exclusion according to features and pricing considerations. Careful consideration and clear, unambiguous guidelines would help streamline this aspect.
MINOCA and Takotsubo Syndrome
A few cardiovascular disorders deserve special mention, either for being new additions to the Universal Definition or for their proximity to MI clinically and ability to exhibit MI-like features. It is extremely important that insurers have a detailed understanding of these disorders in order to take appropriate courses of action for underwriting and claims purposes.
Myocardial infarction with non-obstructive coronary arteries (MINOCA): As the name suggests, this condition fits the Universal Definition of acute MI, yet is identified as having non-obstructive CAD (absence of stenosis > 50%) and no clinically specific cause for acute presentation at time of angiography. MINOCA is present in 6% to 8% of the MI cohort population and is common among females and non-ST segment elevation MI (NSTEMI) patients. Although generally there is a series of disruptions or a dysfunction of a coronary artery (plaque, akin to Type 1 MI) or a coronary spasm leading to MINOCA, it should not be confused with other myocardial disorders such as myocarditis, Takotsubo syndrome, and other cardiomyopathies which are categorized under troponin-positive, non-obstructive coronary artery syndromes.10
To summarize, high troponin levels and normal or non-obstructive coronaries are key indicators of MINOCA. As MINOCA is a relatively newly identified condition with subtle overlaps with other cardiovascular disorders, it would require sophisticated risk assessment and experienced understanding to determine its qualification as MI, as age and gender also play a crucial role. However, the need, at least from a claims perspective, is to focus on the detailed reasoning by the attending cardiologist to ensure the diagnosis of MINOCA as MI.
Takotsubo syndrome (TTS) is another relatively newly defined cardiovascular disorder. With a staggering 90% of cases occurring among post-menopausal women and triggered generally by stress or physical factors, it shows a remarkable similarity to ACS. Inpatient mortality coincides with that of ST-segment elevation MI (STEMI) (4% to 5%). While the ECG changes may be similar in MI and TTS, the ECG changes in TTS are usually not in definable coronary vascular territories.
The rise and fall of troponin levels is indicative of myocardial injury. CAD is present in 15% of TTS cases, which makes the situation more complicated.7
TTS is not considered a part of MI definition despite the fact that some of these will have coronary disease. Although there are some clinical similarities between TTS and both MI and cardiomyopathy, it would be prudent for insurers to treat TTS and MI as individual entities.
Troponin Elevation and Diagnostic Tests
- Troponin factor: A recent article recommends obtaining serial cTn values and comparing them across different intervals for the assays to be reported. However, in reality it is unlikely that underwriters receive a complete set of comprehensive information.8 The article does emphasize obtaining gender-specific 99th percentiles, if available, as bias may prevent underdiagnoses in women and overdiagnoses in men, but does not mandate it. With differential points suggested for evaluation, this opens up a new Pandora’s box in terms of the availability of such tests as well as implications on pricing assumptions. It will definitely have an effect on the current percentage distribution (e.g., gender bias) of a cohort qualifying for MI. Insurers should monitor this closely across geographies and have a focused discussion in order to develop a uniform approach. As of now, insurers depend on hospital or clinic assays, their respective limit ranges, aggregate or gender-specific, to confirm diagnosis of MI and trigger the corresponding claim.
- Diagnostic tests: There is no significant change from a diagnostic perspective from the preceding definitions (ECG changes are only required for diagnosis of MI), but when evaluating a claim from an insurance risk assessment perspective, it is recommended to review more advanced diagnostic tests, if available, to avoid any overlap with other CVDs. Thus, advanced tests such as CMRI or CTCA may become more commonly encountered.
Final Word
The Fourth Universal Definition of Myocardial Infarction, while providing more clarity for the insurance industry, is designed for clinical purposes. The concept of myocardial injury, the varying elevations of troponins related to myocardial injury or otherwise, and the newly associated or related CVDs which may overlap with MI, are well documented. However, the implications of these new definitional factors on the insurance industry are currently less conclusive than might have been anticipated.
Age, gender, and clinical diagnosis, including all related tests (including but not limited to cardiac biomarkers and advanced imaging techniques), must be carefully considered before drawing any final conclusions on a firm diagnosis of MI, as both the psychological and legal implications are profound. Any doubts or suspicion of other cardiovascular disease overlap must be overruled by conducting tests with higher specificity for the same. In countries with limited availability of troponin or imaging techniques, the challenge is more acute and product pricing will vary accordingly.
Furthermore, consideration of the new Universal Definition of MI does raise the question that an update of this magnitude might impact all insurance industry verticals, including costs and global revenues. Is now the right time to collaborate as an industry and form standardized guidelines of inclusion and exclusion, which might help mitigate ambiguity and provide consumer-friendly coverage?