In this Health Brief, we look at the growing utilization of bariatric surgery as a means of achieving rapid weight loss, and consider if it should be covered more widely by health insurance.
Many today view the massive worldwide increase in obesity over the past two-plus decades as a pandemic. The 2013 Global Burden of Disease Study from the Institute for Health Metrics and Evaluation found that from 1980 to 2013, worldwide incidence of being overweight or obese rose by 47.1% for children and 27.5% for adults. Additionally, in 2014, the World Health Organization estimated that about 13% of the world’s population could be considered obese. The combination of more sedentary jobs and lifestyles and over-consumption of calorie-rich processed foods is leading to ever increasing Body Mass Indices (BMI) as well as to a myriad of related health problems such as heart disease, stroke, Type 2 diabetes, and certain cancers.
At its core, the standard treatment regime for obesity remains diet and exercise; i.e., reducing caloric intake and concurrently increasing energy expenditure. These basics are often combined with associated strategies and health services including dietitian/nutritionist services, counselling and support groups, and occasionally weight-loss drugs.
However, as bariatric surgery advances and becomes more common, it is increasingly being used as a quick-fix treatment for weight-related conditions. This article explores the type of patients who may benefit from bariatric surgery, provides an update on the various surgical techniques and their efficacy, gives guidance around verification of medical necessity of treatment, and comments on claims and underwriting considerations.
What Constitutes Obesity Today?
The currently accepted definition of obesity, as outlined by the World Health Organization (WHO), is “a medical condition in which excess body fat has accumulated to the extent that it may have a negative effect on health.” This accumulation is considered to occur due to a combination of excessive food intake, lack of physical activity and genetic susceptibility.
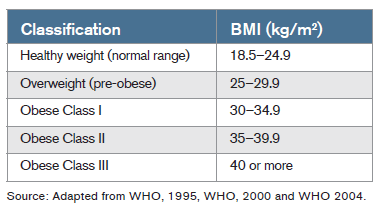
Until the 1990s, serious obesity, at least in the U.S., was defined as weighing at least 45 kilograms (100 lbs) more than the actuarially determined body weight. In 1995, however, the WHO adopted a classification formula based on a ratio of weight to height, the Body Mass Index, as a tool to determine the level of obesity.
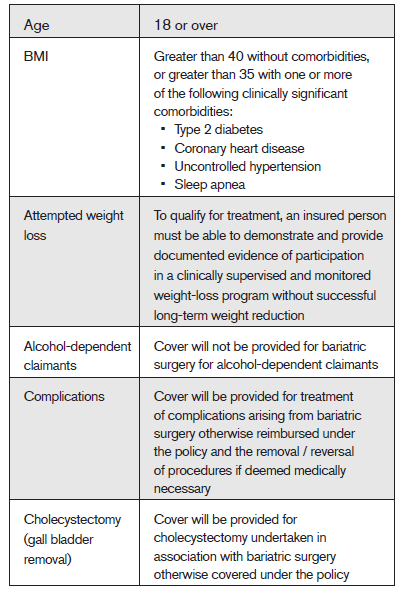
The World Health Organization classifies normal, overweight, and obese BMIs in adults as follows:
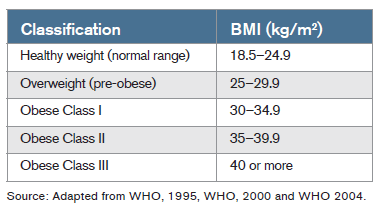
In recent years, additional classifications have been developed in the surgical literature to highlight particularly severe obesity. Those having BMIs of above 50 are considered “super obese.”What is considered “obesity” can also differ from country to country. In Japan, for example, obesity starts with a BMI of 25, and in China, with one of 28.
Patient Eligibility for Bariatric Surgery
Coverage for weight-loss surgery, also known as bariatric surgery, has historically not been provided by the vast majority of health insurance policies, as insurers had deemed it a cosmetic procedure. (The term “bariatric,” which is defined as “relating to or specializing in the treatment of obesity” comes from the Greek words “bari” [or “baros”], meaning weight or heft, and “iatros” [physician] or “iatrikos” [medical]).
Clinicians today, however, are arguing more frequently that given the health risks of obesity, the surgery could be medically indicated for more severe cases. In addition, due to bariatric surgery’s possible complications, it should only be considered for patients for whom there is a clear clinical need.
Coverage for bariatric surgery varies by country. In the countries we examined for this article, government or socially funded surgical intervention was only considered for patients whose obesity could be deemed potentially life-threatening (a BMI of 40 or greater, or BMI of 35 or more and comorbid with a serious medical condition such as hypertension or Type 2 diabetes), and often only when lifestyle modifications (diet and exercise) could be shown as ineffective in reducing the patient’s BMI.
Some funders apply additional eligibility criteria, such as:
- The patient having achieved a target percentage reduction in body weight prior to surgery
- Acceptable documentation proving the patient failed to achieve and/or maintain a beneficial reduction in body weight using non-surgical (diet and exercise) weight control methods
- Requiring a commitment from a patient to ongoing long-term follow-up
- Confirmation the patient is fit enough to undergo surgery and associated anesthesia
There may also be other criteria, such as comorbidities that would automatically exclude individuals who might otherwise meet the above qualifying criteria. These can include advanced cancer, liver disease, a mental health disorder that might limit a patient’s ability to commit to ongoing lifestyle modification, and an alcohol and/or drug dependency.
Finally, bariatric surgery is not normally recommended for children, but may be considered in extreme circumstances for physically mature children (girls approximately age 13 and boys approximately age 15), if they have a BMI (adjusted by age percentile) of more than 50, or of more than 40 and have been diagnosed with one or more serious health conditions.
Types of Surgery
Bariatric surgery results in the patient feeling satisfied after taking in far less food than normal, thereby achieving the goal of weight loss in a shortened timeframe. Four major types of such surgeries are performed today:
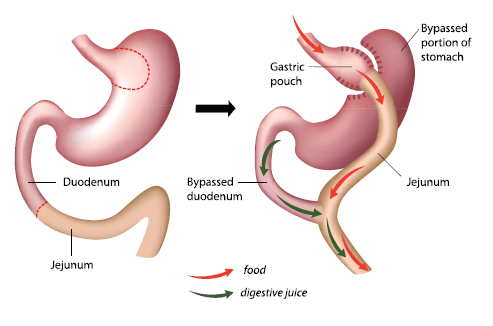
Roux-en-Y gastric bypass
In this procedure, which is the best known and most familiar to the general public, a gastric pouch of approximately one ounce (30 milliliters) by volume is created at the top of the stomach. The pouch is then partitioned from the rest of the stomach either by cutting or stapling. The small intestine is then cut about 18 inches from the stomach. The point of the cut is worked into a “Y” configuration (therefore the name), with one limb attached to the upper pouch, and the other to the remaining portion of the stomach, for drainage. This configuration means both that less food is required to fill the stomach, and the food bypasses the majority of the stomach and the first part of the small intestine. A variation of this procedure, the biliopancreatic diversion (either with or without the duodenal switch), also involves removal of a portion of the stomach and the creation of a gastric pouch, and involves bypassing approximately 75% of the small intestine as well. This procedure, which enables very rapid weight loss, especially in the first few months following surgery, is meant for the severely obese.
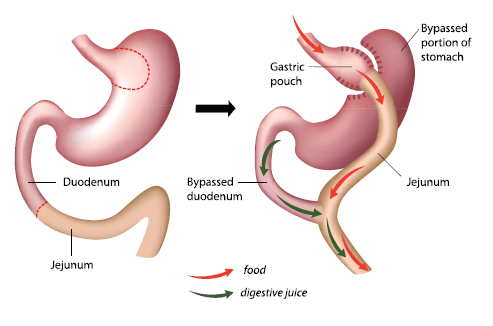
Although the roux-en-Y procedure is performed laparoscopically it is classified as a major procedure and usually requires a two-night hospital stay. The surgery is irreversible, and surgical risks include leakage, blood clots and hemorrhage. Longer-term complications can include hernias, intestinal obstruction, malnutrition, and dumping syndrome.
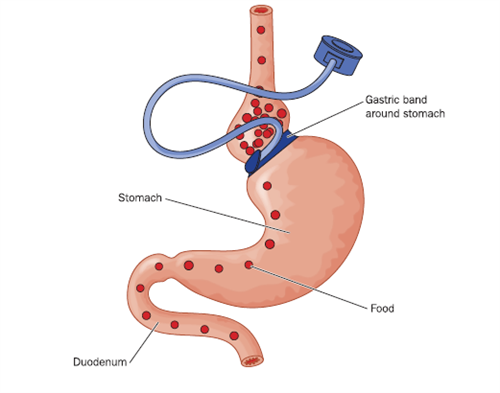
Gastric (Lap) band
In this surgery, the most common bariatric procedure performed in the U.K. today, an adjustable inflatable saline filled silicone band is positioned near the top of the stomach to create a gastric pouch similar in size to that in the roux-en-Y procedure. Although the pouch restricts the amount of food that can be eaten at a single sitting, it also allows food to move to the rest of the stomach and through the entire intestine. The size of the opening between the gastric pouch and the rest of the stomach permitted by the gastric band can be regulated via the injection or removal of saline from the band through a dedicated access port just under the skin. After the band is placed, it is filled over a period of weeks until optimal restriction has been achieved (though not full separation, as food still needs to move into the digestive tract).
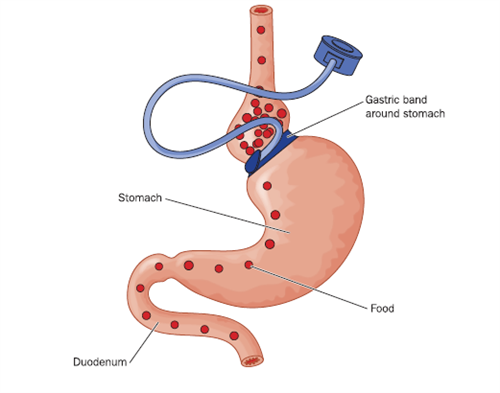
This laparoscopic surgical procedure for lap band insertion is far less invasive than that for a gastric bypass. No cutting of the stomach or the intestine is involved. The procedure is normally performed under general anaesthetic as a day patient. For morbidly obese patients, however, laparoscopic insertion may not be possible.
The band is generally left in place even after the desired weight loss has been achieved, but the patient should be monitored.
This method also reduces the amount of food needed to make the patient feel full, resulting in reduced calorie intake and weight loss. The band will assist the patient in losing weight, but the patient will need to make long-term changes to food consumption patterns in order to maintain the weight loss.
Surgical mortality for gastric band recipients is far lower than for gastric bypass patients. There are also fewer life-threatening complications, but risks can include: infection; internal bleeding; gastritis; and slippage of and leakage from the band. A band left in place over the long term also risks complications such as erosion (the band working its way into the stomach wall), which would necessitate additional surgery.
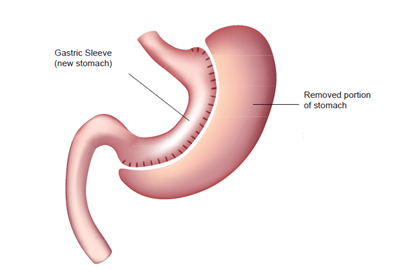
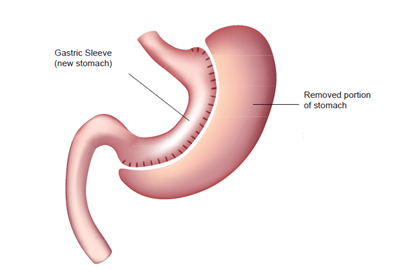
Gastric sleeve / sleeve gastrectomy
In this procedure about 75% of the stomach is permanently removed, leaving the patient with a stomach approximately the size and shape of a banana. Weight loss is achieved due to the reduced size of the stomach, resulting in the patient feeling full after the consumption of less food. No portion of the intestine is excised.
This procedure is normally performed laparoscopically, making it minimally invasive. Its surgical risks can include internal bleeding, infection, gastric or bowel obstruction and internal bleeding. Longer-term complications can include GERD (gastroesophageal reflux disease, or heartburn), gallstones, hernia, and nutritional deficiency.
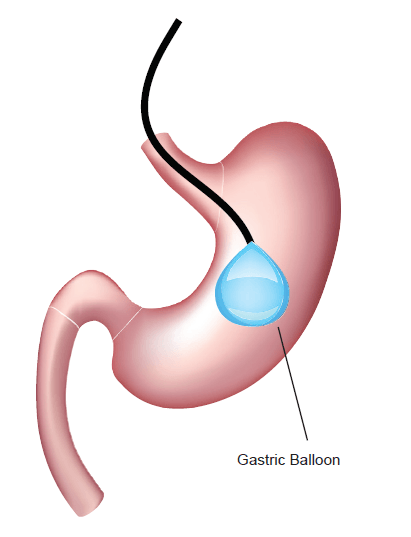
Gastric balloon
This non-surgical endoscopic procedure entails the temporary (maximum six months) insertion of a deflated silicone balloon via the mouth and esophagus. Once in the stomach, the balloon is inflated with saline to about the size of a grapefruit. It is designed to provide a feeling of satiety with less food. The patient generally does not require anesthesia for this procedure but will need sedation.
Patients undergoing this procedure learn to modify the amount of food they require.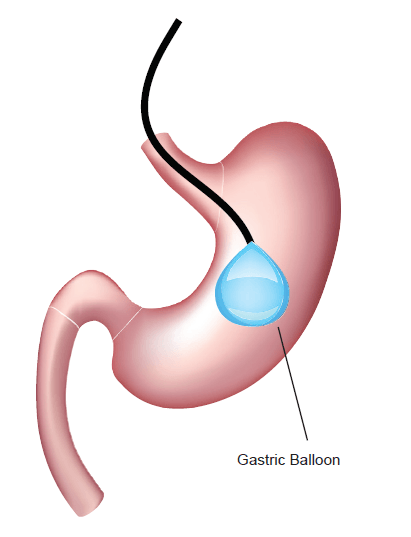 Once the desired amount of weight is shed, the balloon is then removed in the same manner in which it was inserted. Risks are far fewer for this procedure, but
Once the desired amount of weight is shed, the balloon is then removed in the same manner in which it was inserted. Risks are far fewer for this procedure, but
they do exist, and are likely to be gastric problems such as reflux, abdominal pain, nausea or vomiting, faulty balloons leaking or rupturing, or complications from insertion.
Following weight loss, patents who have been obese for long time periods may be left with excess skin. Surgery to remove this excess skin is available, but is considered cosmetic rather than medically therapeutic and is often not covered.
Whatever type of surgery is undertaken, it is only part of the cure for an individual’s obesity condition. Those who wish to maintain a reduced weight will have to modify their lifestyles and reduce caloric intake in the long term.
Claims Considerations
Many health organizations and professionals throughout the world now recognize obesity a chronic disease. We are seeing an increasing number of claims for bariatric surgery, which is being recommended as treatment for weight-related conditions such as Type 2 diabetes and obstructive sleep apnea. Health insurers need to consider each individual request for cover against the particular policy benefits, terms and conditions applicable for the claimant. Claims assessors, when considering a claim for bariatric surgery, will also need to verify the claimant made a full and accurate disclosure at the time of application, including height and weight.
When considering a claim for bariatric surgery that is represented as treatment for weight-related conditions, the insurer will need to consider the items listed below:
Is the condition or its treatment excluded?
Health insurance policies normally contain exclusions that disallow cover for specified conditions or bariatric surgery. Common exclusions include “cosmetic or aesthetic surgery” and sometimes “treatment relating to obesity,” and these exclusions have been used to deny cover for weight-loss surgery. However, as this type of treatment is becoming more commonly recognized as a treatment protocol for other weight-related conditions, it is becoming harder for insurers to rely on this type of exclusion. We have seen regulators and ombudsmen affirm that if the purpose of the surgery was to positively impact a covered condition even if weight-loss surgery was excluded, and did have a positive impact, then the insurer should pay for the surgery.
If an insurer has not priced to cover such treatment and therefore wishes to exclude it from cover, the exclusion will need to be clear and specific and not restricted to treatment of a particular condition such as obesity. (Sample exclusion language: “We do not cover bariatric surgery undertaken for any reason.”)
Is the treatment “medically necessary” as defined by the provider?
Treatment reimbursed under health insurance should meet a good policy definition of “medically necessary.” Such a definition should only allow treatment that adheres to evidence-based current best treatment protocols. An insurer may wish to rely on comparing each treatment request against current treatment protocols to decide if it meets the definition of “medically necessary” (as they should for all claims). RGA is seeing specialist health insurers set out clear guidelines for when they will cover such treatment.
The definition provided for “medically necessary” should ensure that all treatment received is undertaken in accordance with current standards of medical practice and does not allow the medical provider to:
- Over-treat the patient
- Undertake treatment purely for their or the patient’s convenience
- Use a more expensive procedure than one that
provides the same therapeutic results
Each company will want to develop its own “medically necessary” guidelines for bariatric surgery, which should be centered on evidence-based clinical best practice. Guidelines may include:
Each claim would need to be considered against the guidelines, which insurers may choose to publish, but insurers need to be aware that there may be claimants with circumstances not covered by the guidelines which will need to be considered. Such cases will again need to be assessed against current evidence-based clinical best practice.
Bariatric surgery has been used for treatment of conditions in non-obese patients. For example, the roux-en-Y gastric bypass is sometimes used to treat GERD. If an insurer finds clinical evidence in support of such treatment and decides to provide cover they should include details of what conditions and circumstances would qualify for such treatment in their guidelines.
Unproven bariatric surgical techniques or interventions should not be covered. Company medical officers should ensure that they keep up to date with latest clinical practice and update the underwriting and claims guidelines as new techniques become accepted as standard clinical practice.
Underwriting Considerations
If an applicant for health insurance discloses they have previously had bariatric surgery underwriters will want to see details of the applicant’s height and weight both before and after the procedure, and will want the applicant to be at least 12 months after successful surgery with stabilized weight before accepting them for cover. The first five years post-surgery will still require an additional rating in addition to any rating for current build. An applicant who is longer than five years post-surgery with a stable weight and build may be able to be accepted with rating based only on their current build.
If more insurers decide to provide cover for bariatric surgery, the cost of the treatment and aftercare will need to be factored into premiums. That may be at least partially offset by savings in not having to cover treatment of weight-related conditions.
Conclusions
Obesity is an increasing problem in many parts of the world and a direct cause of certain major non-communicable diseases that are reaching pandemic proportions.
These diseases are giving rise to a material proportion of medical treatments, the costs of which are covered by many health policies. Bariatric surgery is now recognized as a treatment for non-communicable conditions caused by obesity, and is becoming more commonly used.
The cost of bariatric surgery may be lower than the cost of ongoing treatment for weight-related conditions that would otherwise be covered by health insurance. To provide clarity to policyholders and avoid conflict at the time of claim, insurers should decide if and under what criteria they will cover bariatric surgery, make this information available to their policyholders, and price their products accordingly.



 Once the desired amount of weight is shed, the balloon is then removed in the same manner in which it was inserted. Risks are far fewer for this procedure, but
Once the desired amount of weight is shed, the balloon is then removed in the same manner in which it was inserted. Risks are far fewer for this procedure, but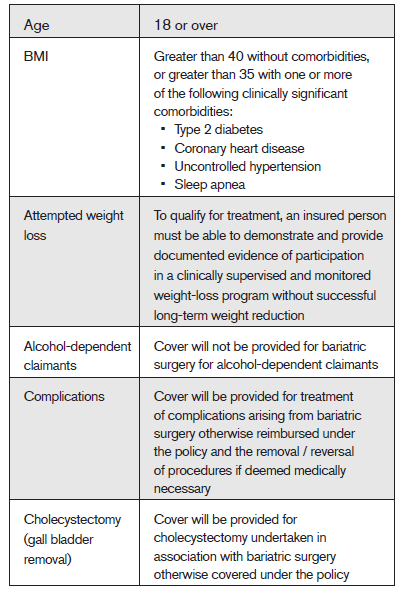
3b6df65b-f107-43ac-9b32-d8a308104d95.png?sfvrsn=8a342d60_3)