The biological behavior of the novel SARS-CoV-2 virus is both fascinating and perplexing.
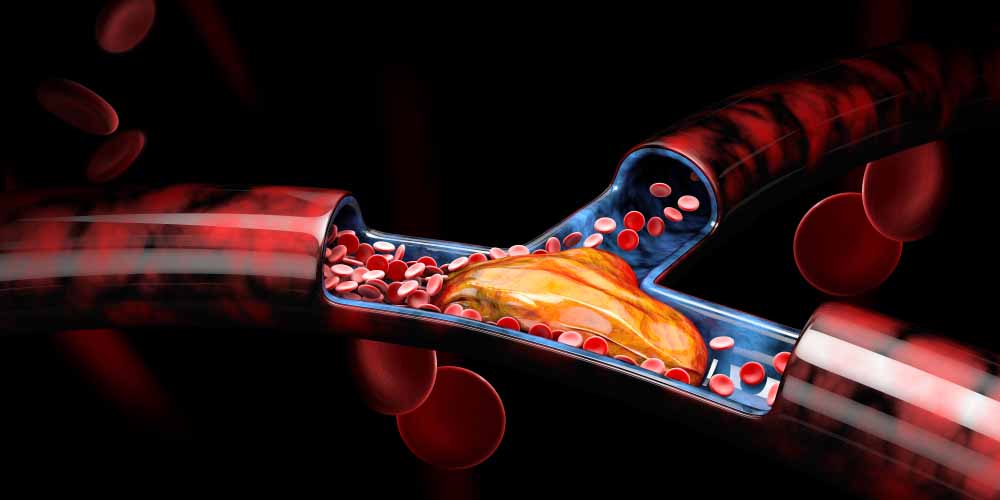
One of the incompletely understood findings in early published clinical case series studies from various geographies, especially in critically ill patients as well as autopsy findings, is a hypercoagulable state (increased clotting of blood) and the predisposition to thrombosis.1, 2, 3
The term COVID-19-associated coagulopathy (CAC) has been coined.
Venous thromboembolism, including deep vein thrombosis and pulmonary embolism, as well as arterial thrombosis – although less prevalent – have been reported. Pulmonary embolism is the most frequent thrombotic complication.2 On the other hand, bleeding complications in patients with COVID-19 appear to be uncommon.4
Abnormalities in coagulation parameters including elevated fibrinogen and D-dimer, with minimal change in PT (prothrombin time), aPTT (activated partial thromboplastin time), and platelet count paint the typical clinical picture of CAC in hospitalized COVID-19 patients in the early stage of the infection. While such findings are associated with a high risk of thrombosis, a sudden drop in fibrinogen and platelet counts later in a disease course may signal the development of acute disseminated intravascular coagulation (DIC), where bleeding is the major outcome. Although a distinct clinical entity, DIC can also complicate severe COVID-19 infection.
Coagulation studies have shown a normal or slightly prolonged aPTT which measures the intrinsic (blood vessel related) clotting pathway and might indicate an increased risk of bleeding.
The significance of this observation is still not completely understood, and in a small case series from the U.K., the lupus anticoagulant, which leads to an artifactual prolongation of the aPTT, was found in 91% of patients.5 This finding, as well as any mild thrombocytopenia, should not, however, according to the authors, preclude the use of anticoagulation prophylaxis.
Significantly elevated D-dimer levels (a protein fragment produced when a blood clot dissolves) have been found on testing, along with the observation that higher levels appear to predict mortality.4 The American Society of Hematology (ASH) advises that a normal D-dimer is enough to exclude the diagnosis of pulmonary embolism, but that an increased D-dimer in the context of a congruent clinical picture (and mindful that symptoms of pulmonary embolism overlap with COVID-19), requires additional imaging to exclude or confirm the diagnosis of a pulmonary embolism.6
The necessary components for hypercoagulability are present in all severe infections namely immobilization, endothelial damage, and excess circulating prothrombotic mediators – and COVID-19 is no exception. And even despite clotting prophylaxis interventions, the risk of thrombosis remains high in the latter group. Microvascular thrombosis has been observed in the lungs and may explain why some people experience critically low blood-oxygen readings and why mechanical ventilation has been of varying benefit.7 The microvascular thrombosis is seen in an environment of marked inflammatory changes.
Arterial thrombosis involving the central nervous system, heart, and limbs has been reported.8 Of note in a relatively small U.S. case series and uncharacteristic of the usual presentation of a stroke, is this presentation occurring in younger patients (all were under age 50) with relatively mild symptoms and the disproportionate involvement of the large central nervous system vessels.9 Large vessel involvement in this and other series in more severely affected individuals has also prompted support for thromboprophylaxis in patients.2
What seems to be the underlying mechanism leading to a hypercoaguable state?
Although still a mystery, one hypothesis is that the virus can enter endothelial cells (those lining blood vessels) through the same angiotensin converting enzyme 2 (ACE2) receptor that the virus uses to enter lung cells. Inflammatory damage to the endothelium by proinflammatory cytokines and chemokines, possibly aggravated by the lack of any prior acquired immunity, together with a down-regulation of ACE2 results in unopposed angiotensin II effects. This results in vasoconstriction, fibrosis, inflammation, and thrombosis.10 At the same time, the infection is also associated with a remarkable activation of the fibrinolytic system and plasminogen activators, explaining the high levels of D-dimer and fibrin degradation products.11 Cytokines also increase the liver’s production of clotting factors. And, when co-morbidities like diabetes and hypertension are present, the impact is compounded.
Is this unique to SARS-CoV-2?
A relationship between infections and thrombosis has been shown in previous cohorts of critically ill patients. Whether this is more significant in COVID-19 is currently unknown, but data are emerging to suggest this may well be the case. In a small single center series from France, 22 of 107 (21%) confirmed COVID-19 patients admitted in ICU with pneumonia were found to have pulmonary embolism as opposed to 6% and 8%, respectively, in two matched cohorts – one from the same time interval in the previous year and the other from ICU patients with influenza rather than COVID-19.12 This suggests a two-fold higher incidence of pulmonary embolism with COVID-19 infection.
Why is this relevant?
1. Preventing, identifying, and treating CAC is crucial to the prognosis of people infected with COVID-19.
Optimizing patient care in order to impact clinical outcomes is a crucial part of minimizing the impact of this novel pathogen. Management, however, is challenging as with many other aspects of the care of COVID-19 patients owing to the lack of high-quality and randomized evidence. Additionally, antithrombotic therapies carry bleeding risk which must be offset and individualized, particularly in those who are already on anticoagulation for other indications, e.g., atrial fibrillation.
- As for all coagulopathies, treatment of the underlying condition is paramount; however, the impact of COVID-19-specific therapies on thrombotic risk is unknown at this stage and clinicians need to be mindful of any possible drug-drug interactions.
- Current guidance, unless contraindicated, is for all hospitalized patients with COVID-19 to receive thromboprophylaxis with low molecular weight (LMW) heparin (except where there is renal dysfunction) or unfractionated heparin.13,14
- Full therapeutic dose anticoagulation is required for established deep vein thrombosis or pulmonary embolism.
- The use of tissue plasminogen activator (tPA) is still advocated where indicated for limb threatening DVT, massive pulmonary embolism, and acute stoke, or myocardial infarction.
- Plasma exchange has been postulated to be of benefit, although this is considered experimental at the current time.11
- Any bleeding complications would be managed in the same way as in non-COVID-19 infected patients.
With regard to underwriting risk, it is suggested to discuss the following cases with a medical officer:
- If there is uncertainty when assessing an applicant with a history of CAC or a particular thrombotic outcome or about prophylactic or therapeutic treatment doses.
- If someone remains on anti-coagulant therapy for longer than the expected period.
- If prescribed treatment suggests any underlying coagulopathy.
- Recovered applicants may well be discharged on anticoagulation treatment as the risk of thrombosis in high-risk groups was quoted as high as 60% of patients having clots in the 90 days after discharge.15
2. It is critical to understand the possible impact of COVID-19 on morbidity outcomes.
The interplay between inflammation and coagulation may be an important pathway to COVID-19-related multiorgan injury. The associated impact on morbidity and possible longer-term sequelae is an evolving area which we will need to continue to carefully monitor given the impact on the range of additional insurance products that are offered in different markets, including critical illness and disability.
Summary
Together with other potential indirect impacts on health caused by COVID-19 as well as the furious pace at which knowledge is being acquired, RGA remains committed to staying abreast of new developments. This includes carefully following emerging evidence regarding COVID-19-associated coagulopathy.