While the number of COVID-19 cases is starting to decrease in certain countries around the world, experts suggest that the COVID-19 pandemic will be a long-term crisis, needing long-term solutions. But what will eventually end the crisis?
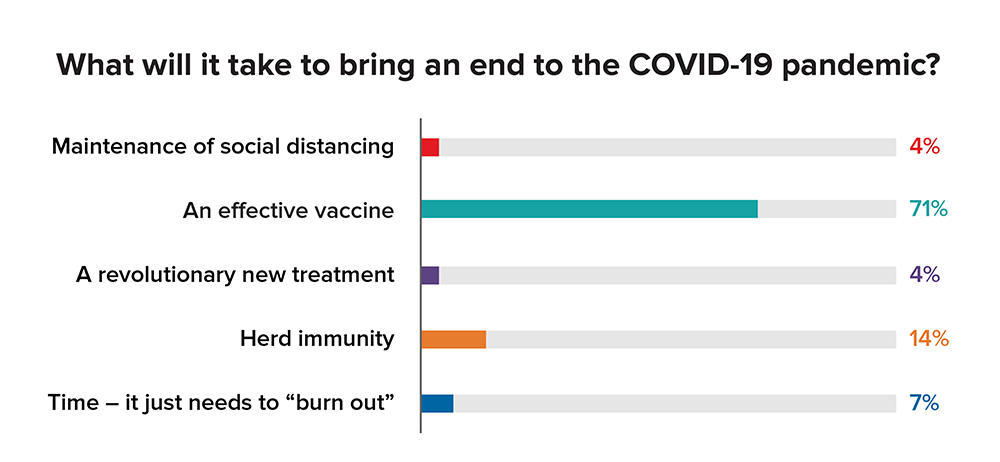
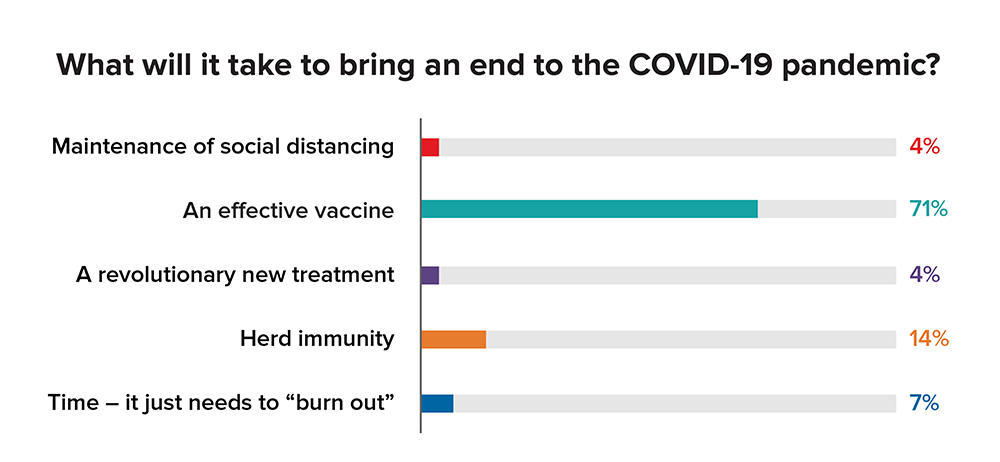
Based on results from a live polling question during the recent webinar "The COVID-19 Pandemic: Insights and Implications for Insurers", most respondents (71%) believe that an effective vaccine is needed to end the pandemic, followed by herd immunity (14%). While both of these factors weigh very heavily and are, in fact, closely related, the likely answer is that all of these components will play an important role in our fight against the virus.
Maintenance of social distancing
Social distancing appears to have been effective in areas where implemented and some governments have started to test multi-cycle “suppression and lift” strategies. Currently, guidelines and stay-at-home orders differ worldwide and we’re closely monitoring the outcome of reopening strategies. The deployment of technology, such as contact tracing via mobile phone applications and data collection, may also prove to be epidemiologically successful.
Herd immunity
To prevent sustained transmission of COVID-19 and achieve “herd” immunity, around 70% of the population needs to be immune to the infection. Despite the rapid spread of the virus so far, the current exposure rate may be only in the single digits. Continued natural infection, unfortunately, and the expeditious development of a vaccine, hopefully, will be needed to lead to herd immunity.
An effective vaccine
According to reports, the earliest that a vaccine could be rolled out is by September 2020; however, a 12-18-month timeline remains more realistic for vaccine development – especially in large quantities. While prior research, ongoing collaboration, financial support, and novel technologies may help accelerate the timeline, other stages such as safety trials and production are more fixed.
Furthermore, to achieve herd immunity, we will need to commercially produce vaccines on the scale and time span that makes it viable. However, not everyone responds to vaccines the same way: Older individuals, who are more susceptible to COVID-19, often do not respond to vaccines as well younger people. Additionally, the ongoing anti-vaccination movement may have an impact, as well. If a large number of people refuse to take the vaccine, it will impede the achievement of herd immunity.
A revolutionary new treatment
Researchers across the globe continue to seek treatments for COVID-19, studying the effects of existing medications, convalescent plasma, and other antivirals. While some findings might seem promising, study results overall need to be interpreted with caution as many are neither peer-reviewed, nor placebo-controlled.
We continue to monitor research findings in this area, including the work of several former grant recipients of the Longer Life Foundation, a collaboration between RGA and Washington University School of Medicine in St. Louis.
Time – it just needs to “burn out”
While time, natural variation, and possible regression of the virus may play some role in ending the pandemic, this should not be assumed to be the case. Certainly, more will be learned about this factor with time.
Summary
While it’s too early to tell which approaches to COVID-19 will prove to be most effective, it’s clear, in one way or another, multiple factors will play a role in the fight against the pandemic. Life and health insurers need to closely monitor developments in all areas and continue planning for the long-term impact the coronavirus will have on our business and practices.
At RGA, we are eager to speak with clients about any support needed as we confront this challenge together. Click here to view the full webinar, and contact us to learn more about the resources, solutions, and services available.