BPA and disease development
Reproductive system disorders
BPA is known to have adverse effects on human health, especially the reproductive system. It can cause pathological changes in the placenta and obstetric complications, such as decreased fetal growth, miscarriage, pre-term birth, and pre-eclampsia. Additional adverse effects include endometrial hyperplasia, development of ovarian cysts, and infertility. According to the World Health Organization (WHO), the global lifetime infertility prevalence estimates from 1990-2021 were 17.5%, or approximately one in six people experiencing infertility in their lifetime.13 Many experts have associated this high rate with higher exposure to BPA.
Studies indicate a relationship between increased levels of BPA in men and their semen quality/infertility,14 with fetal exposure to BPA known to affect the quality and quantity of sperm.3 In some regions, recorded sperm counts have declined by as much as 50% over the past 50 years.1
Mothers with higher BPA plasma concentrations risk a shorter pregnancy duration or premature rupture of membranes.14 In fact, pre-term birth rates in the US have risen by more than 30% since 1981. In 2020, the pre-term birth rate in the US was 10.0%, which was higher than the global average of 9.9%.15 By 2022, the US rate rose to 10.4%, the highest figure in 10 years.16 The risk of mortality and morbidity in pre-term infants increases according to the degree of prematurity.
Cancer
Research connects BPA to the development of hormonal-related cancers, such as breast, ovarian, and endometrial cancer. BPA binds to estrogen receptors, such as Erα and Erβ, which are expressed in more than 60% of human breast cancers. The abnormal expression of estrogen receptors leads to the development of breast, ovarian, and low-grade endometrial cancer.
In addition, studies show that BPA can cause resistance to well-known chemotherapy drugs, including doxorubicin, cisplatin, carboplatin, tamoxifen, bevacizumab, PARP inhibitors, and vinblastine.7
BPA also influences the development of male cancers, such as prostate cancer and testicular germ cell cancer, and has been linked to the development of acute myeloid leukemia, lung cancer, colorectal cancer, hepatic cancer, head and neck cancer, thyroid cancer, and osteosarcoma.3 In 2022, over 1.8 million cases of cancer were diagnosed in the US, which had one of the highest age-standardized incidence rates worldwide at 303.6 cases per 100,000 population.17
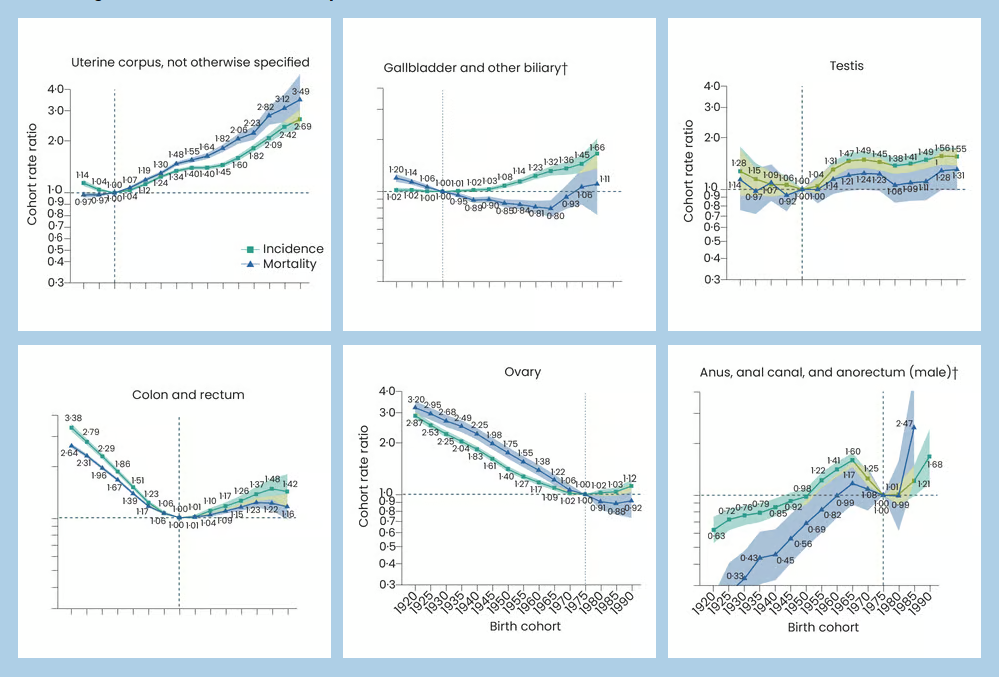
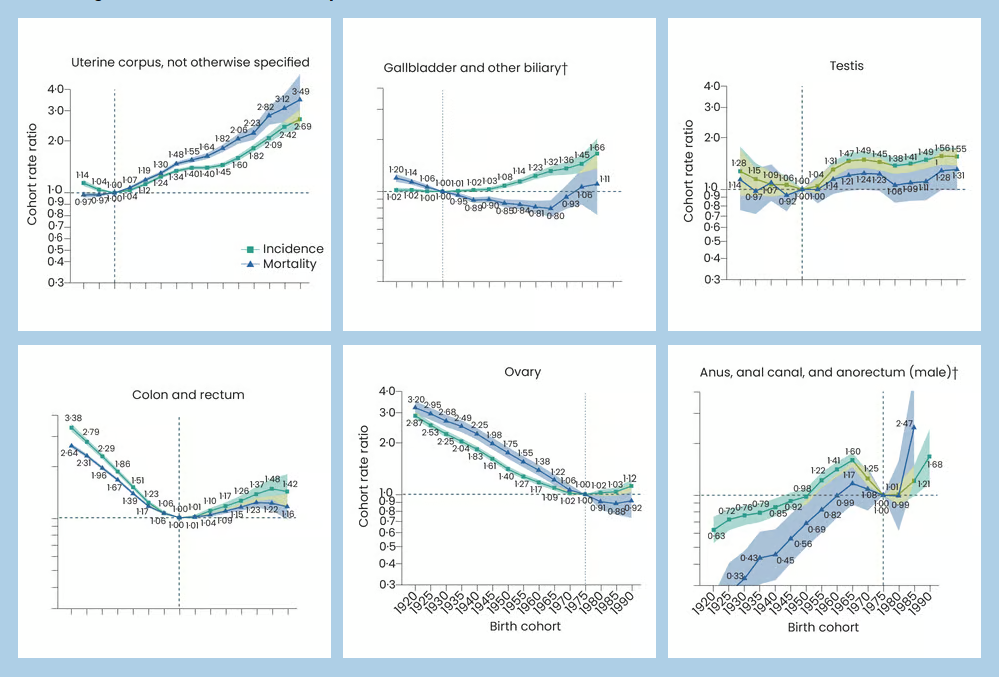
According to a 2024 analysis examining differences in cancer rates of US adults born between 1920 and 1990, 17 out of 34 cancer variations experienced increasing incidence in younger birth cohorts. Of these 17 cancers, nine had previously shown declining incidence in older birth cohorts, including estrogen-receptor-positive breast cancer, uterine corpus cancer, colorectal cancer, ovarian cancer, and testicular cancer. This may reflect exposure to carcinogenic factors during early life compared to older generations, as well as an increasing incidence in obesity rates. Indeed, the fastest rise in obesity rates has occurred in those aged 2-19 years. Suspected risk factors for the rise in cancer rates among young lives include unhealthy diet, sedentary lifestyle, and exposure to environmental chemicals in early life.18
Figure 1: Birth cohort incidence and mortality rate ratio trends from 1920 to 1990 for six cancers with reversing trends in incidence compared with older birth cohorts in the US from 2000 to 201918
Neurodevelopmental and childhood disorders
Neurobehavioral disorders represent EDC exposure’s largest health impact in the US.
Gestational exposure to BPA interferes with pre-natal brain development while increasing the risk of attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD), depression, poor language development, sleep disorders, and uncontrolled behaviors, including aggression, destruction, and hyperactivity.1
Mothers with high BPA concentrations were 3.7 times more likely to give birth to sons with a low language score. Autistic children have shown heightened oxidative stress due to increased exposure to BPA, while ADHD was found to be more common in formula-fed infants in 2007. Infant exposure to BPA has decreased in recent years with the introduction of regulations banning its use in baby bottles and infant formula packaging.4
The prevalence of developmental disabilities in US children increased from approximately 13% in 1997 to 17% in 2022. Concerns have emerged regarding the increasing prevalence of ADHD, where the percentage of children aged 4-17 years with ADHD rose from 7.8% to 9.5% between 2003 and 2007, a 21.8% increase.19
Pediatric cancers are also a concern. Children under the age of five have experienced increasing incidence of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), ependymal tumors, neuroblastoma, and hepatoblastoma.20 Neonatal or early-life exposure to BPA is a risk factor for developing prostate cancer in later life.
Other disorders
Research indicates that BPA plays a negative role in thyroid disorders, non-alcoholic steatosis, osteoarthritis, inflammatory bowel conditions, alteration of the gut microbiome, obesity, diabetes, cardiovascular disease (CVD), and neurotoxicity.21
While there are some known lifestyle causes – such as poor diet and lack of physical activity – that contribute to increased diabetes and obesity rates, EDCs are understood to have a significant impact by promoting metabolic dysfunction. Initial studies show that BPA can cause changes in human blood glucose levels and insulin resistance, while increased urinary BPA levels in adolescent children have been positively associated with metabolic syndrome.14 Metabolic-disrupting chemicals have also been linked to the abnormal growth of fat mass, which causes weight gain by altering the endocrine system responsible for metabolism and appetite.1
The association of BPA with all-cause and cause-specific mortality risk
Although studies to date suggest BPA exposure increases the risk of all-cause and cause-specific mortality, this association is difficult to prove and quantify without deliberately exposing humans to these chemicals and examining the results. However, some studies do support this association:
- A study using NHANES data (2003-2016) showed that the highest tertile of urinary BPA levels, when compared to the lowest group, was linked to a 36% increase in all-cause mortality, a 19% increase in cancer mortality, and a 62% increase in CVD mortality. A low urinary BPA level and high dietary quality had the lowest all-cause and CVD mortality (HR 0.42 and 0.30, respectively).21
- In another study using NHANES data (2003-2008), when comparing the highest and lowest urinary BPA levels, all-cause mortality in adults age 20 and older was HR 1.49, while CVD mortality was HR 1.46.22
- In a study of nearly 9,000 patients with hyperlipidemia, all-cause mortality was 20% higher among the highest tertile of urinary BPA vs. the lowest group.23
Conclusion
BPA has emerged as a significant public health concern. Over the past two decades, the incidence of female and male reproductive disorders has risen rapidly, as have the rates of neurobehavioral disorders in children and certain cancers. The consumption of, and exposure to, BPA is purported to have significant consequences for future generations worldwide and contribute substantially to disease and reduced lifespan.
You need a partner with the financial strength, global reach, and local insights to help you with your life and health risk. Learn more about RGA today.