The humble Cannabis sativa plant, cultivated for millennia for its psychoactive properties and more, is today considered one of the most controversial and complex plants in the world.
Starting in the early to mid-20th century, much of its use became recreational, but by the early 1970s discoveries began to emerge around its potential medical efficacies.
This article will discuss current knowledge of how cannabis engages with the brain and the endocannabinoid system (ECS) and provide an overview of the new market landscapes brought about by changes in governing laws and regulations, which are affecting usage by our current and potential customers. It will also explore the additional hazards, concerns, and considerations of cannabis use in countries where it remains illegal.
Introduction
Naturally occurring psychoactive substances have been part of human life for millennia. One of the most frequently utilized plant sources of these substances, Cannabis sativa, is also the best-known worldwide. For the past half-century, scientific and medical interest in its many compounds, known as cannabinoids, has been increasing. Today, the two best-known, delta-9 tetrahydrocannabinol (THC), its psychoactive chemical, and cannabidiol (CBD), which does not have psychoactive properties, are some of the most commonly used in the world.1
Laws and regulations governing cannabis – both its products and its use – differ from market to market. Although possession and use are still illegal in most of the world’s countries, many do not enforce their laws. Several of the world’s developed countries have decriminalized and even legalized medical and, in some cases, recreational use.
In Canada, for example, cannabis has been legal for medical use for nearly 20 years and for recreational use since October 2018, and today it is widely available.1 In the U.S., however, cannabis possession and use continue to be illegal on the federal level. The U.S. government maintains cannabis’ classification as a Schedule 1 substance under the Controlled Substances Act. (Schedule 1 drugs are considered to have high potential for abuse and no currently accepted medicinal use.) Still, conditional legalization for medical cannabis use exists in several U.S. states as well as the District of Columbia, and a few states have even legalized it for recreational use.
In South Africa, cannabis use has been decriminalized, but commercial cultivation and sale remains illegal. Medical use is legal in Australia as well but is subject to qualifying conditions by state, and recreational use has mostly been decriminalized and is legal in some states for personal use. In India, both medical and recreational use are illegal, but bhang, a traditional edible cannabis preparation commonly used in Hindu religious ritual and in Ayurvedic medicine, is excepted.
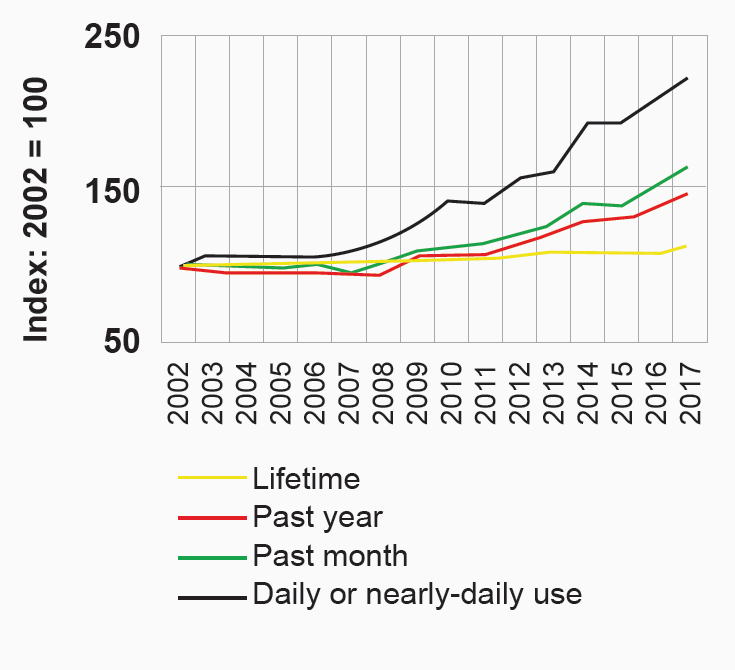
Figure 1
U.S. cannabis use trends, age 18 and older, 2002-2017
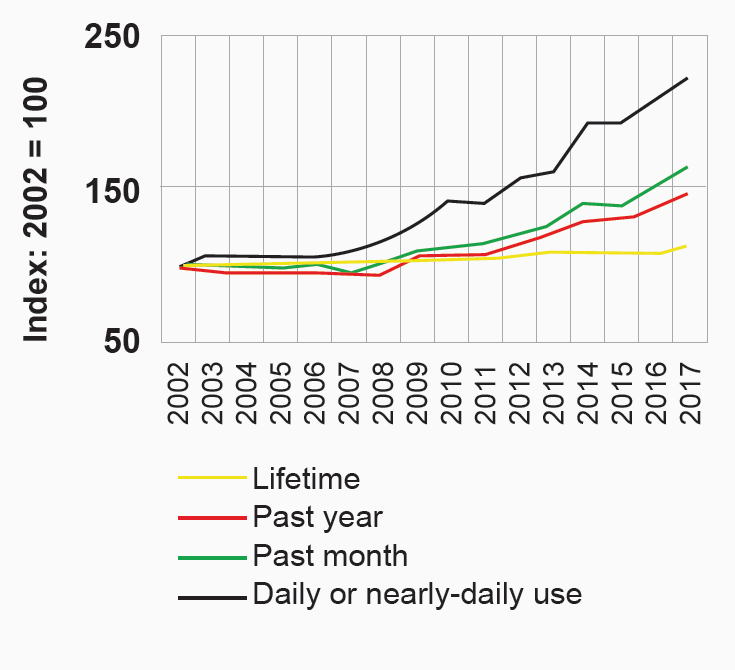
Source: United States, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, Results from the 2017 National Survey on Drug Use and Health: Detailed Tables (Rockville, Maryland, 2018).
As research into cannabis and its compounds proceeds, new discoveries are being made about potential pharmacological efficacies. At the same time, prevalence of use is continuing to grow worldwide, and its legal status is evolving as well. Because of this, the insurance industry needs to stay up to date on research, governing laws and regulations, and how they are impacting market characteristics.
Prevalence of Use
Today, an estimated 188 million individuals worldwide use cannabis, according to the European Drug Report 2019.1 Prevalence of use varies in accordance with location, age, gender, and sociodemographics. It is important to recognize that prevalence of use is high in countries where cannabis is still illegal. Clearly, it does not need to be legal to be used.
In Asia, the highest prevalence of use is found in India and Pakistan, most likely due to consumption of bhang. Prevalence of use in Europe ranges considerably, from 7.4% among adults ages 15-64 to 14.4% among younger adults (ages 15-34). Among younger European adults, prevalence of use also varies widely from country to country. In Hungary, for example, where cannabis is illegal for any use, 3.5% of younger adults are users, whereas in France, where recreational use is illegal but certain cannabis-derived medical preparations are legal, young adult prevalence of use is 21.8%.2
What are the additional challenges and hazards in regions where cannabis use and/or possession is still illegal, and what has been observed in countries where it has been legalized or decriminalized?
Two lessons from markets with populations indicating more experience with cannabis use are that prevalence of use appears to increase in response to legalization or decriminalization, and the demographics change. In the U.S., for example, individuals age 18 and older indicating daily or near-daily use of cannabis doubled between 2002 and 2017.1
In the past, cannabis use was associated with certain population characteristics, with average users being young adults, and greater use was reported among males than females. The easing of laws and regulations governing cannabis over the past few decades has been creating new user demographics. Data from the Canadian Survey on Cannabis shows that the number of female and older users is high and rising. Seniors (age >65 years) have the most growth in cannabis usage – a 10-fold increase since 2012. In addition, according to the survey, more than 400,000 seniors were using cannabis by the end of 2019. Increased cannabis use among these older adults has also contributed to a rise in the average age of cannabis users in Canada, from 29.4 in 2004 to 38.1 in 2019. Most of the seniors are new users who purchase it for medicinal purposes and from legal sources.3 Among younger adults (ages 15-24), however, use is mainly recreational, and for those in the 45-64 age group, motivation for use is almost equally divided into recreational, medicinal, and mixed-use.
How is the mixed-use category defined? Is cannabis used to treat serious medical conditions or minor ailments? Is it done under medical supervision?
Even though cannabis is more widely accepted today than ever, most healthcare professionals are still not comfortable authorizing it. Most times, medical cannabis use is patient-driven. In Canada, cannabis is not prescribed as it has no drug identification number (D.I.N.); rather, it is authorized by physicians. There is also no detailed drug information, no official monograph, and it does not come with clear recommendations in terms of initial dose, titration methodology, or proper use. The authorization form provides some guidance, such as “start low and go slow,” that the initial dose should not be not more than 0.5-1 g/day, and that the maximum authorized dose is 3 grams of dried plant/day and up to 25 mg THC/day.4 This information can certainly generate polarizing conversations, drive further analysis, and does not provide much comfort when insurance applicants are underwritten, especially those who are regular cannabis users.
The cannabis world is evolving rapidly, its legal landscape is changing, the prevalence of use is increasing, and the insurance industry needs good data to guide risk stratification. For example. based on a 2016 Clinical Reference Laboratory study which tested 574,541 insurance applicants during the period of 1995-2014 for the presence of THC-COOH metabolite, the prevalence of cannabis use in the U.S. insurance applicant pool was quite substantial. It ranged from 1.1% in female non-smokers to 14.8% in male smokers. The latter approaches the prevalence reported in the U.S. general population in 2017.8 Newer data confirms that cannabis test positivity is climbing in the general U.S. population. In 2009, it was reported that 2-3% of all drug tests and across all employee testing categories showed positivity for cannabis, an almost 17% increase since 2014.9
Does all this information mean cannabis is ready for prime time? Some believe it might be a universal remedy – the new super-drug. Others, however, are skeptical of the many claims for its efficacy. Most users seek it out for the chronic pain triad: physical pain, mood disorder (anxiety and depression), and insomnia. Often it is self-prescribed rather than authorized or recommended by a physician.
People with severe medical conditions, such as cancer patients, may prefer it over opioids for pain relief. This is one good reason cannabis should be clinically studied. Indeed, scientists are actively researching this complex plant, which has hundreds of chemical entities, with more than 800 ongoing studies.
Cannabinoid Science
Scientists first isolated THC and CBD, the two best-known cannabinoid molecules, in the 1960s. In the years since, research has determined cannabis to have some medical efficacy, such as easing interocular pressure from glaucoma and reducing chemotherapy-induced nausea. However, only in the 1990s did researchers begin to understand how cannabis exerts its effect on the body and brain.
In 1996, scientists discovered the body’s own natural cannabinoids—anandamide (AEA) and 2-arachidonoyl glycerol (2-AG). These two chemicals, called endocannabinoids, along with their receptors, make up the endocannabinoid system (ECS). Indeed, research into the effects of the two major cannabinoids led to the discovery of the ECS and its function.16 This fascinating system plays a critical role in regulating mood, pleasure, memory, thinking and concentration, body movement, awareness of time, appetite, pain, and the five senses.
The two ECS receptors found thus far, CB1 and CB2, are located throughout the body. CB1 receptors are found mainly in the brain and central nervous system and are in many peripheral organs as well, and CB2 receptors are found primarily in the immune system.
AEA is a neurotransmitter secreted by the brain and is the body’s own version of exogenous THC. The name “anandamide” comes from the Sanskrit word ananda, which means bliss. AEA and THC molecules are very similar, which is why AEA is also called the natural THC, or bliss, molecule.
The breakthrough discovery of AEA broadened science’s understanding of how cannabis exerts its effect. AEA’s close relationship with dopamine may explain its important role in mood regulation.15 Dopamine is released by the brain when experiencing pleasurable activities and as a reward for behavior that, historically, has improved humanity’s chance of survival. As the reward system uses AEA to release dopamine in small amounts, AEA directly affects energy, mood, sleep, appetite, and more.
Does more THC mean more dopamine? Not long-term. As THC resembles AEA, habitual cannabis use disrupts the AEA-dopamine cycle by frequently signaling for dopamine release. If excessive dopamine levels continue, the brain’s dopaminergic receptors downregulate. This is the reason chronic cannabis users need increasingly more potent products (as well as more frequency of use) to achieve the same effects.14
Is Cannabis Safe or Hazardous?
The growing importance of the ECS is now recognized in human health and well-being. While cannabis use is not without risks, scientists agree that there is no risk of lethal overdose from plant-based cannabis products. The reason is the neuroanatomical distribution of cannabinoid receptors. While ECS receptor concentration is high in the frontal cortex, amygdala, basal ganglia, and cerebellum, which are the brain regions involved in learning, emotion processing, and body movement, concentration is low in the brain stem. Opioids and alcohol can impair the respiratory and circulatory systems, which are located in the lower brain stem, but cannabis does not have the ability to affect this critical area of the brain. In addition, cannabis has a very large therapeutic index (TI). The TI of a drug is the ratio that compares the blood concentration at which a drug becomes toxic and the concentration at which the drug is effective – the larger the TI, the safer the drug.12
Therefore, while one can overdo cannabis intake, as is commonly seen with edibles, it is not possible to die from a cannabis overdose.13
Does this mean cannabis is safe for medical use? That is still unknown. Insufficient high- quality studies, addiction risk, and lack of reliable information about its interactions with other medications and side effects are important challenges, but lack of user knowledge is a prime reason for concern. The known health hazards of cannabis can be moderated through a user’s behavior and choices. Cannabis products from illegal sources may be highly potent and not quality-controlled and properly labeled, and their use brings additional challenges.
Available literature attests that frequent or intensive (i.e., daily or near-daily) cannabis use is strongly associated with higher risks of experiencing use-related adverse health and social outcomes, and higher risks of various acute as well as chronic problematic mental and behavioral outcomes.10, 11
However, with new legislation and wider acceptance, the profile of cannabis users might change. More people may use it for milder medical conditions such as anxiety, depression, back pain, and insomnia. Medical cannabis users also tend to buy the products legally, whether from dispensaries or online, in order to access higher-quality products in more reliable doses.
Motivation of use is also changing: for many newer users it is not to get high but to assist their ability to recover from underlying conditions. The risk of graduating from cannabis to harder drugs is lower as the newer providers have a broad range of choices. Also, shopping at a dispensary allows relationships to develop. The purchase is less about the user getting what they want than it is about someone listening to their problems and offering solutions that meet their need.
Because of all these factors, the risk profiles of newer medical cannabis users are likely better than in the past. Assuming no other unfavorable risk factors, these individuals might actually have better risk profiles than recreational users. However, the insurance disability risk might be higher due to the underlying condition(s) for which the medical cannabis is being used.
In addition, available studies thus far have produced controversial results, so the individual perspective on cannabis will guide how the evidence of benefits and harms is viewed.
Health hazards attributable to cannabis use depend on the individual users, their health profiles, and the company their usage keeps, e.g., whether they use alcohol and/or other illicit drugs, driving criticism, and overall high-risk behavior
As cannabis is now legal (or at least decriminalized) in many markets, this extraordinarily complex plant must continue to be scientifically studied and assessed. Cannabis is clearly not a mono-molecule: it consists of numerous compounds which can and do interact in unexpected and sometimes opposite ways, and their effects are yet to be determined through high-quality studies. Cannabis falls into the category of substances which are tolerated and discouraged at the same time. Knowledge is key, and awareness is power. The potential harms can be mitigated by collaborating and knowledge-sharing to increase awareness surrounding the nature and composition of cannabis products.
Cannabinoids vs. Opioids
Could cannabis be a safer alternative than opioids for patients with chronic pain?
The growing interest in cannabinoid science may be a collateral effect of the opioid epidemic. Available U.S. research from 2014 and 2019 found a 25% decrease in opioid overdose death rates reported in states permitting medicinal cannabis use versus those that did not.5, 7 In addition, a 2017 survey demonstrated that 69% of older adults (ages 50-80) in the U.S. believed that cannabis provides pain relief and 70% believed its side effects were tolerable compared to those of opioids.6
Today
Is cannabis yet ready for prime time?
Cannabis plant products affect users in different ways, depending on the type of product used, the interaction between the product and the user’s brain chemistry and genetics, and the motivation for use.
While attending the first Canadian cannabis conference, this author underwent pharmacogenetic testing to determine how THC was personally metabolized and the risk for cannabis-related health hazards. The results showed normal (or average) metabolism. These tests seem to support the theory that not everyone is affected in the same way.
Cannabinoid science is surely captivating and is generating substantial and increasing interest. Research into its many compounds is still in the early stages, but esteemed universities are currently running hundreds of studies to understand the pharmacological properties of this controversial plant and determine its risks, hazards, and possible benefits.
The ECS seems to play an essential role in both health and disease. Cannabis-derived drugs that interact with the ECS could have important therapeutic applications if used with medical supervision. Unfortunately, there could also be severe adverse consequences.
Today, many therapeutic interventions are available for people with chronic pain. However, before resorting to a drug-only therapy, remember that humans can recalibrate their minds and bodies in natural ways. For example, balanced levels of dopamine and AEA, which are responsible for mental and emotional health, can be stimulated in natural, healthy, and safer ways, through items as simple as laughter, exercise, healthy food, yoga, mindful meditation, and music.
A growing body of research has started to provide evidence of the pharmacological potential of cannabis on a wide range of disorders. But it should be recalled that motor vehicle accidents are a prime reason for early mortality risk, and that any drug that mimics a substance naturally produced by the body could affect us in ways that are yet to be completely understood.
Information about cannabinoids and the ECS gathered from scientific study will surely help insurers underwrite applicants who are regular users of cannabis, whether medically or recreationally.