While cardiovascular disease is the leading cause of death globally, more men and women are surviving heart attacks than ever before. As a result, insurance claims assessors may expect to see more living benefits claims for heart attack. Another potential contributing factor is the reported increase in heart attacks among those under 40 due to poor lifestyle choices, lack of exercise, unhealthy diets, smoking/vaping, and substance abuse.
Following a heart attack, an insured can make a claim on a variety of benefit types, including death, disability, and medical reimbursement, but the most common heart attack claim is for critical illness (CI). Understanding exactly what happens when an insured has suffered a heart attack is crucial for claims assessors managing CI claims.
What Happens During a Heart Attack
Payment of CI benefits is not dependent upon a heart attack diagnosis, but upon meeting a specified definition of “heart attack,” which is usually contingent on the size of the infarction suffered and the resulting myocardial damage. CI definitions of heart attack typically require a specific presentation, identifiable symptoms, and evidence of severity measured during cardiac investigations, which may be explicitly defined.
When assessing such a CI claim, it is important to be familiar with the typical series of events that occur during a heart attack. This information can help determine exactly what clinical evidence will be available and help the assessor appropriately direct claim enquiries.
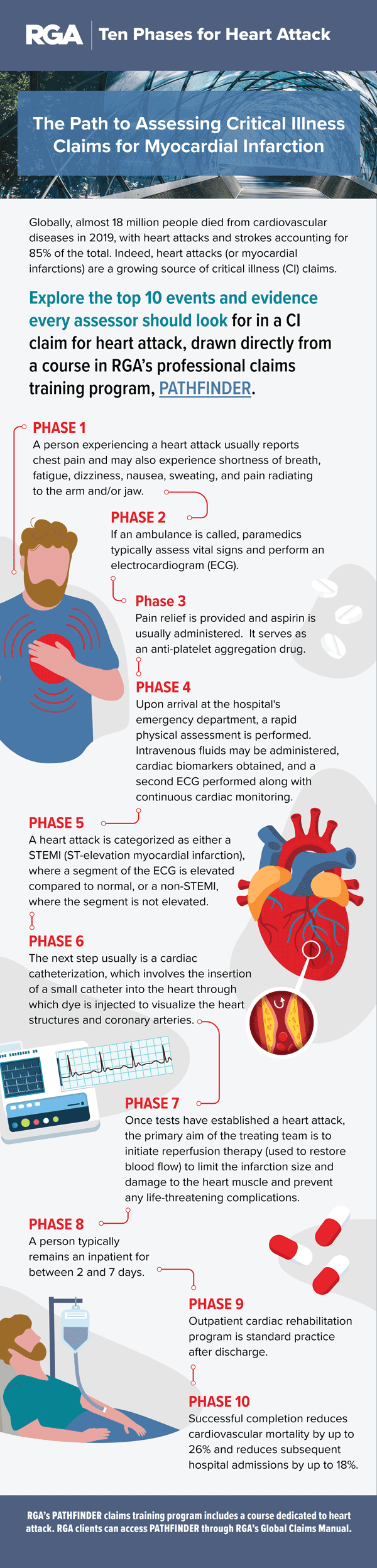
Ten Phases of a Heart Attack
A heart attack occurs when the flow of oxygen-rich blood to the heart muscle is restricted or blocked. The heart muscle does not receive enough oxygen and begins to die. While the most common cause is coronary artery disease, many different factors can contribute to heart attack such as trauma to blood vessels, hypoxia, or even drug misuse.
Note: These steps are provided as an example. Not all heart attacks will follow this exact presentation. The infographic shows an overview of the typical presentation and treatment of a heart attack.
With a STEMI diagnosis, which is where the artery or arteries are completely occluded, surgical reperfusion (Phase 7), is usually commenced quickly, ideally within 90 minutes of presentation. This is likely to involve percutaneous coronary intervention (PCI) or angioplasty/stenting. In more extreme cases, coronary artery by-pass graft (CABG) may be required to address arterial blockages. With NSTEMI, which is where there is some limited remaining blood flow, treatment is dependent on multiple factors, including underlying comorbid conditions and the degree of stenosis.
Typically, cardiac biomarker tests are repeated several times after hospital admission, and these test results can support the insurance claim assessment. Troponin levels are expected to increase within three to 12 hours from the onset of chest pain, peak at 24-48 hours, and then return to baseline over the next five to 14 days. It is important to note that troponin levels may not be detectable for up to six hours after the onset of an infarction, so abnormalities may not be detected in the initial reading conducted upon admission. If ECG findings and the clinical presentation are significant, a patient may be taken straight to cardiac catheterization/surgery before the troponins are available. Typically, however, testing is conducted beforehand.
Standard practice after hospital discharge is to refer the patient to an outpatient cardiac rehabilitation program to support recovery, reinforce positive lifestyle changes, and help prevent another heart attack.
Claims Considerations for Heart Attacks
- Not all heart attacks show up on the first ECG. If an ECG has been performed only upon initial arrival at the emergency department or while in transit in the ambulance and the result does not provide clear-cut evidence of an infarction, the possibility of a heart attack should not be ruled out. An ECG performed within a few hours of the onset of heart attack symptoms may return a normal reading and demonstrate no evidence of an infarction. Understanding the ECG readings provided and the specific timeframe within which the ECGs were performed are therefore of equal importance.
- Similarly, when relying on cardiac biomarker testing, it is essential to consider when, during the patient’s presentation, the testing was conducted and whether the insurer has appropriate access to the results of all biomarker testing performed over the period of admission. Very early or very late cardiac blood tests may not demonstrate evidence sufficient for the insurer’s purposes. Troponin levels typically peak between 24-48 hours after initial onset of heart-attack symptoms.
- Commonly, as soon as a blockage(s) is identified, the patient is fast-tracked to percutaneous coronary intervention (PCI)/angioplasty to restore blood blow to the heart. It is important for claims assessors to understand when this procedure occurs. If it happens prior to when cardiac biomarkers would have been expected to peak, it may not be possible to demonstrate a rise and fall or elevation of troponin to a specified level, which is often required by heart attack policy definitions. In this scenario, the relevant angiography report can be discussed with a chief medical officer to determine how troponins would have reacted, based on the degree of blockage/stenosis in the arteries.