Quick: describe what you do in fewer than 30 seconds. It’s not easy, is it?
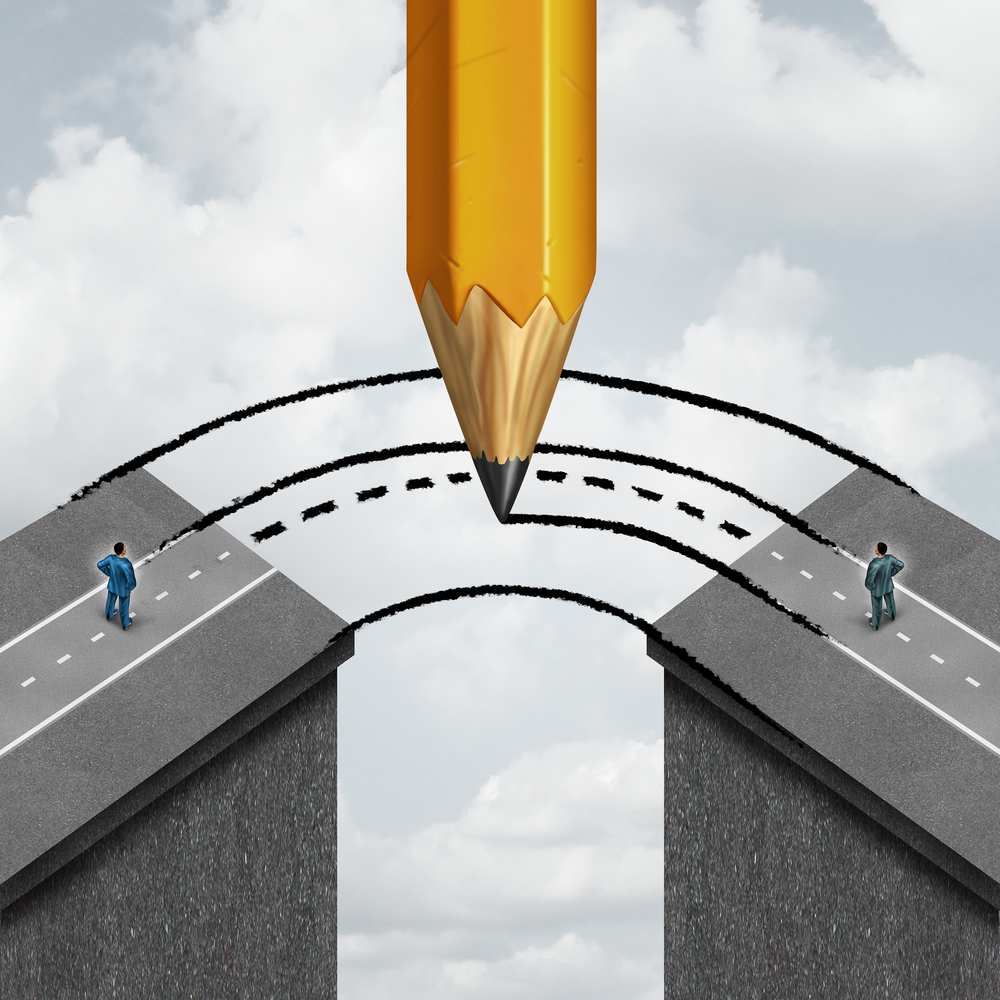
Many of us struggle to explain our roles. Yet effective teamwork is based on strong, two-way communication and an equally powerful appreciation the contributions of other team members.
Underwriters and claims analysts should work as a team, but too often we operate at cross purposes.
What stands in the way? We have much in common. Both positions require highly trained experts with deep experience and sound judgment. Yet underwriters and claims analysts also play distinct roles with significantly different responsibilities, reporting relationships, and even vocabularies. A simple communications failure can cascade into a misguided renewal, while persistent breakdowns can build into bad blocks of business. To succeed, every member of an insurance team must overcome differences to properly write and adjudicate policies. As an underwriting team, we have seen our share of mixed messages and missed opportunities due to miscommunication.
The Underwriting Picture
The very nature of the insurance process can place underwriters and claims analysts at odds. After all, while underwriters assess the risks, claims analysts must respond when those calculations go wrong. When a flood of claims come in, claims analysts might ask “What were they thinking?” They might also accuse underwriters of being overly dependent on automation.
Underwriting requires critical thinking – not just keystrokes. No matter how skilled, the underwriter rarely has all the information, but must instead synthesize multiple data sources and actuarial inputs to draw the best possible conclusion. This is an art as much as a science.
Three key factors help complete the picture:
- Risk Assessment: In assessing the risk of any particular group, underwriters start with the basic assumption that past performance is a good indication of future risk. The underwriter sifts through data looking for any unexplained or unusual patterns, potential large claims, and changes in the financial strength of the counterparty to gain a sense of what unites the employee populations in the case of several companies applying under a multi-employer group.
- Pricing: Underwriters make decisions that could be very profitable or very costly, depending on their precision in pricing. They consult actuaries and manuals to price risk, evaluate varying geographic and demographic trends, look for shifts in administration or provider contracts, and explore factors such as aggregate claims, large claim history, contract types, and overall expenses and profits.
In a competitive marketplace, underwriters are often under pressure to price before conducting a full risk assessment of a group. By the same token, at renewal time, assumptions made last year about the employee population may no longer be valid.
- Packaging: Few third-party administrators (TPAs) or brokers welcome the potential for a rate increase. It is important to recognize that market forces often mean that underwriters must choose between the price they want and what can be sold. In group underwriting, much depends upon how a proposal is packaged and whether the decision maker, broker, or TPA happens to be an advocate. As stop-loss and other group products become commoditized, insurers everywhere are seeking to avoid becoming another column on a spreadsheet. The underwriter needs to be looking for opportunities to differentiate a proposal from the competition.
The Claims Perspective
Underwriters should understand that no claims analyst has a crystal ball and communicate accordingly. For example, it is not uncommon for an underwriter to approach a claims counterpart to ask how much a particular claimant will cost next year.
This question frustrates many claims analysts due to a simple misunderstanding. Underwriters communicate in categories and generalities, grouping risk into severe, moderate, and minor cost ranges. In this scenario, the underwriter may be attempting to gauge if the claim will range from $30,000 to $50,000 or if the cost will reach $100,000, $250,000, or more. In contrast, claims analysts are expected to deliver specifics. The analyst can easily, although mistakenly, assume he or she is being asked to predict the future precisely to the penny for a complex claim event that has not yet occurred. Simple clarification at the outset could prevent significant wasted effort.
Underwriters and analysts can benefit by talking to each other more frequently, especially regarding more challenging cases. Underwriters can highlight accounts for claims counterparts to watch, and analysts can share significant claims trends and the potential for a certain diagnosis to lead to complications. An ongoing dialogue between these groups can prevent surprises, preempt bad renewals, and deliver real results.
Lost in Translation
“Communication is key” is more than just a cliché. The proper use of words and phrases can unlock a wealth of meanings. But what happens when the terms in common use carry slightly different definitions in underwriting and claims contexts?
We underwriters use words that have meaning only to us and may not reflect the precise clinical terminology familiar to claims personnel. For example, we might use the term "stem cell transplant", when the claim examiner would consider this term obsolete. Or we may continue to refer to cancer treatment as “chemo” even when new biologics are being used to treat a claimant.
Underwriters and claims analysts, at times, appear to be speaking different dialects of the same language. The danger, of course, is that two individuals could easily walk away with completely different perceptions of the same conversation.
If miscommunication seems like a blueprint for conflict, the remedy is straightforward:
- Ask for clarification whenever information is subject to interpretation; and
- Summarize meetings with shared notes. Recognize, too, that underwriters may not have realized that a medical definition has changed. Suggestions from a claims analyst to adjust the case notes can protect the insurer from potential liability.
Ultimately, underwriters and claims analysts are on the same team, and everyone wins when all team members work together.